$20 Billion Scam At The Heart Of Medicare Advantage
In May of 2023 The $20 Billion Scam At The Heart Of Medicare Advantage, PNHP, Matthew Cunningham-Cook and Andrew Perez, Lever News, May 2023.
Health insurance company Humana enjoyed a banner year in 2022. Humana made $2.8 billion in profits in 2022, while paying out $448 million in dividends to shareholders, and paying more than $17 million in compensation to its CEO.
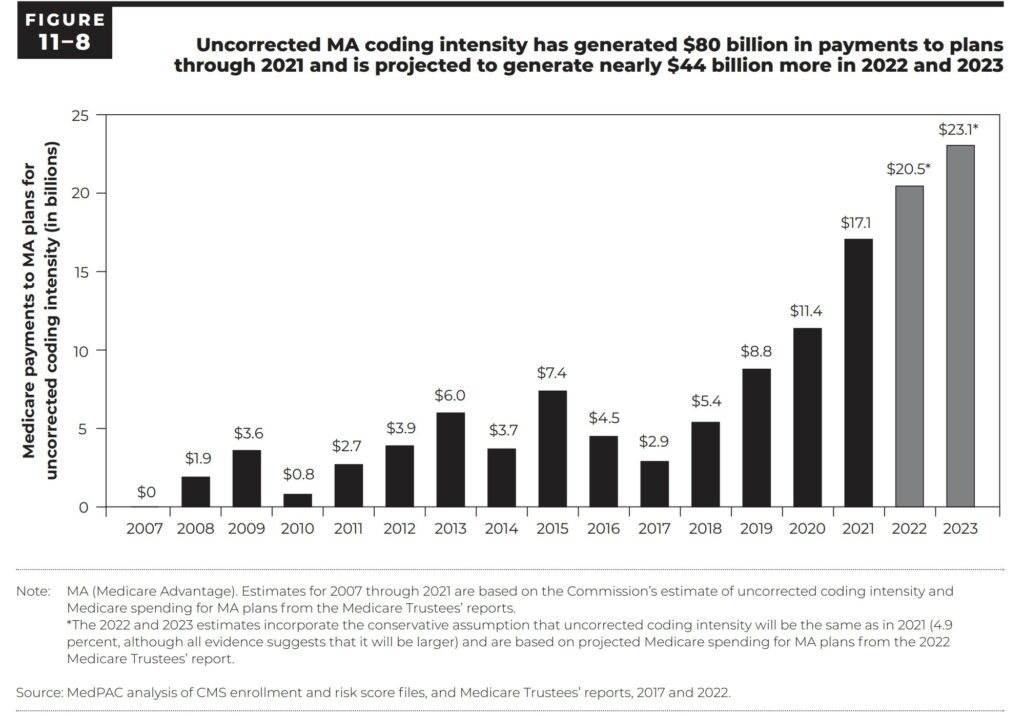
One of the main inputs to those earnings was the federal government’s $20.5 billion in overpayments to Humana and other private Medicare Advantage insurers. These private MA manage their insurance plans on behalf of seniors and people with disabilities. If not for the CMS authorized overpayments, Humana could have suffered an ~ $900 million loss in 2022 (Lever Analysis).
Humana is an example of how insurers built a major cash cow out of systematically overbilling Medicare Advantage. Much of the overbilling was the result of over coding, denial of services, delay of care, etc. plus the CMS percentages added to the charges by the Medicare Advantage plans. The overpayments are symptomatic of a broader profit-driven policy agenda seeking to privatize Medicare. Corporate entities like Humana advertise special programs such as healthcare clubs, dental and eye care, etc. at similar costs to which CMS adds a percentage to the charges to compensate for the additional services. Services which are not allowed for Medicare to offer.
Medicare Advantage plans have higher claim denial rates and more prior authorization restrictions than traditional Medicare plans. Last year, regulators found that nearly one in five payment requests rejected by Medicare Advantage plans in 2018 were wrongfully denied, representing an estimated 1.5 million claims.
MedPAC March 2023 Report to the Congress: Medicare Payment Policy
Industry-Wide and Sponsor-Specific Estimates of Medicare Advantage Coding Intensity, Richard Kronick, F. Michael Chua :: SSRN
2023-Annual-Report.pdf (chiamass.gov)
MedPAC, March 2023 Report to the Congress: Medicare Payment Policy, Page 354 (graph)
The federal government spent $20.5 billion overpaying Humana and other private insurers for the Medicare Advantage plans they manage on behalf of seniors and people with disabilities. If not for those overpayments, Humana could have suffered a nearly $900 million loss in 2022, according to a Lever analysis.
Humana is the most prominent example of how insurers have built a major cash cow out of systematically overbilling Medicare Advantage, the private Medicare program operated by private interests. These overpayments are symptomatic of a broader profit-driven policy agenda that seeks to completely privatize Medicare, one of the nation’s most popular social programs, and lock program recipients into subpar private insurance plans, even when they get sicker and need the best care possible.
Humana sues feds over Medicare Advantage risk adjustment changes, fiercehealthcare.com, Paige Minemyer, Sep 1, 2023 (below).
Humana has filed suit against the feds, saying the Biden administration’s bid to claw back overpayments in Medicare Advantage (MA) is built on “shifting justifications and erroneous legal reasoning.”
Earlier this year, the Centers for Medicare & Medicaid Services (CMS) finalized a hotly anticipated rule that would overhaul risk adjustment data validation (RADV) audits, which determine whether MA plans were overpaid. In a win for insurers, the agency elected not to backdate these audits beyond 2018.
However, CMS did nix the so-called fee-for-service adjuster, which payers argued was critical to ensuring parity between traditional Medicare and MA. The adjuster accounted for errors in Medicare data that the industry argued could lead MA plans to be underpaid.
CMS determined in the initial pitch for a RADV overhaul, proposed in 2018, that the adjuster was not necessary. It maintained that stance in the final rule, arguing that it was backed up by a 2021 court decision that said the adjuster had no mathematical basis.
Lots or reading and references. Enough said. . .

Ah, private enterprise!
This alone looks like a pretty good argument for a UK-style healthcare system, maybe.
So, where is Kaiser in all this mess?
https://www.nytimes.com/2023/09/14/business/ftc-drug-patents-inhalers.html
September 14, 2023
Common Patenting Tactic by Drug Companies May Be Illegal, F.T.C. Says
Experts say the exploitation of a loophole in the patent system has contributed to high prices for inhalers.
By Rebecca Robbins
The Federal Trade Commission on Thursday issued what amounted to a warning to pharmaceutical companies about the legality of a widespread patenting strategy that experts say has helped keep inhaler costs high for patients with asthma and lung problems.
In a policy statement unanimously endorsed by the agency’s commissioners, the F.T.C. said it “intends to scrutinize” whether companies are illegally engaging in an unfair method of competition when they exploit a regulatory loophole that can delay rivals from entering the market.
The policy statement did not single out any particular products. But an F.T.C. official who was not authorized to discuss the agency’s findings said that the agency’s staff had identified dozens of patents on inhalers that appear to be being used in violation of federal law.
“This seems to be a real problem, and one that could really be contributing to unaffordable medicines and drug products,” Lina Khan, the F.T.C. chair, said at a public meeting on Thursday.
At issue is a maneuver in which drug companies patent different aspects of their products and list those patents in a federal registry known as the Orange Book. The listing can be worth hundreds of millions of dollars for a company because it deters rivals from introducing competing generic products. Under certain circumstances, a listing automatically bars federal regulators for over two years from approving a competitor’s generic product.
Only certain types of drug patents — such as those protecting a medication itself or a method of using it — are allowed to be listed in the Orange Book. But that hasn’t stopped companies from listing their patents on inhalers, injector pens and other devices. Those patents sometimes don’t mention the medication they’re delivering. Some are far removed from the world of drug development, like patents for a container, a rubber strap and a dose counter that keeps track of the number of puffs that a patient has left….
American healthcare-provider-private-insurer abuse seems endless and the results are frightening:
https://fred.stlouisfed.org/graph/?g=15a9v
January 15, 2018
Life Expectancy at Birth for United States, United Kingdom, France, Germany and Italy, 2017-2021
https://fred.stlouisfed.org/graph/?g=15a9P
January 30, 2018
Infant Mortality Rate for United States, United Kingdom, France, Germany and Italy, 2017-2021
The distressing point of these important healthcare posts and articles is that American health outcomes are shockingly poor compared to other developed countries. This general problem sorely needs to be resolved.
https://fred.stlouisfed.org/graph/?g=14JS5
January 15, 2018
Life Expectancy at Birth for United States and European Union, 2000-2021
https://fred.stlouisfed.org/graph/?g=14JSe
January 30, 2018
Infant Mortality Rate for United States and European Union, 2000-2021
Possibly there is a need to think about just what rights are we to consider fundamental in this country. Should there be a right to healthcare? Canadians and the British and French would answer, “yes.” Do we agree?
I think we are particularly bad at resolving when our hearts say yes and our head says no.
When someone ends up in the emergency room soon after saying “look at this”, we think perhaps he should pay for it. But then he sues another party for making his stunt look attractive.
We also insist on our right to spend our money on useless stuff. Once we have decided we like snake oil, we don’t want to hear that it isn’t covered.