Private Equity and Hospital Acquisitions
This is another extension of what happens when private equity gets involved in business. Hospitals are more important as it has an impact on the neighborhoods around them. If one dies, the local neighborhood is stranded. Good article on just that topic.
Private Equity and Its Hospitals, Washington Monthly, Merrill Goozner
“Safety net hospitals” serve communities like those in Delaware County, Pennsylvania. Finance companies serve themselves.
If you want to know what happens after a private equity firm plunders one of its hospital acquisitions, visit Delaware County in southeast Pennsylvania. Earlier this month, Crozer Health laid off 215 workers, or 4 percent of the workforce, at its four hospitals in the suburban Philadelphia county amid reports it is late paying its bills, including rent on its hospitals.
Crozer’s owner is a privately held company, Prospect Medical Holdings, headquartered in Los Angeles. Prospect Medical’s purchase of Crozer in 2016 was financed by Leonard Green & Partners, which is an L.A.-based private equity firm with over $70 billion worth of assets in its portfolio that siphoned nearly a half billion dollars from Crozer in the last half-decade.
In addition to the new layoffs, Crozer announced plans to end drug and alcohol treatment at its 313-bed flagship teaching hospital in Chester, a small city in Delaware County some 20 miles from downtown Philadelphia. Chester is over 70 percent Black, with high poverty, unemployment, and substance abuse rates after decades of deindustrialization.
Those moves came after two years of Crozer cutting services. Last fall, the Pennsylvania Department of Health cited inadequate staffing at Crozer’s facilities and ordered it to close its emergency room at 168-bed Delaware County Memorial Hospital in Upper Darby, the second largest hospital in its system. Before the closure order, Crozer had shuttered the facility’s maternity ward, a severe blow in a small city of 85,000 that’s over a third Black and where 75 languages are spoken in the public schools.
Faced with the Pennsylvania Health Department order, Crozer CEO Anthony Esposito—the fifth chief executive officer installed by Prospect Medical in three years—ordered the shutdown of all in-patient care at the hospital, leaving only its out-patient services. The county immediately challenged the move in court as a violation of the original 2016 agreement when Prospect Medical bought the previously non-profit Crozer-Keystone Health System. That agreement included Prospect Medical’s promise to keep all hospitals in the system open for at least 10 years.
“For decades, Delaware County Memorial has been the hospital of choice for that community,” said Frances Sheehan, president of the Foundation for Delaware County, which provides grants and services to community organizations promoting public health. “People walked to the hospital. They walked to their doctor appointments. Having an E.R. up and running was critically important for an aging population. This was a major, major blow to the community.”
Prospect Medical refused to comment for this story through a spokesperson at Blanco + Hopkins & Associates, LLC, a Los Angeles-based public relations firm representing the company.
Cutbacks and closures at community hospitals in low- and moderate-income communities have become routine in the United States. Most are in large cities, inner-ring suburbs, and rural areas with older populations, stagnant incomes, and rising health care needs. Many of these non-profits are called safety net hospitals because most of their clientele are on Medicare and Medicaid, uninsured, or struggling financially.
Some safety net hospitals survive by merging into larger non-profit systems. But a growing number of them have been gobbled up by private equity firms, often interested in making outsized profits and cashing in on their investment quickly rather than maintaining health care services in underserved communities. An estimated 38 percent of the nation’s 5,200 community hospitals are now under private ownership compared to 20 percent a decade ago.
Prospect Medical’s acquisition of Crozer with financial backing by Leonard Green offers a textbook example of how private equity extracts wealth from struggling health care systems. It often does so in ways that leave the health care systems more vulnerable to the financial headwinds they already face. When the 2016 acquisition of what was then known as Crozer-Keystone Health System was announced, Prospect assumed $260 million in debt and pension liabilities for the 6,000-employee company, which had posted operating losses of over $40 million in the previous two years.
Prospect promised state regulators that it would keep its four hospitals open for at least 10 years and its ancillary facilities open for at least five. “Prospect will make significant capital investments in the Crozer-Keystone system, increasing the ability of Crozer-Keystone facilities to modernize, attract more patients and expand services,” a spokesperson told The Delaware County Daily Times at the time.
But the financial engineers at Leonard Green, which held the majority equity stake in Prospect Medical, had other ideas. In July 2019, Prospect executed a $1.55 billion sale and leaseback deal with Medical Properties Trust, a publicly traded real estate investment trust headquartered in Birmingham, Alabama. The arrangement covered Prospect Medical’s hospitals in Pennsylvania, Connecticut, and California.
Prospect’s statement to Medical Properties Trust investors when the deal was announced echoed its claims made earlier to state and local officials in Pennsylvania. Samuel S. Lee, CEO of Prospect Medical . . .
“This transaction allows us to unlock the value of those assets and focus our efforts on our core business of operating hospitals and implementing our coordinated-regional-care population health model. Having Medical Properties Trust available for long-term capital provides us with a significant and experienced potential source of funding for improvements to our existing facilities.”
Prospect Medical did use some of the proceeds to pay down debt. According to an analysis by the public-interest group Private Equity Stakeholder Project, almost half of the $457 million was used to pay dividends to Prospect’s shareholders at Leonard Green. Meanwhile, individual hospitals in Prospect’s system were saddled with huge rents with so-called escalator clauses for the buildings they used to own. In other words, they were saddled with new debt.
In Crozer’s case, the rents totaled $35 million a year, according to Sheehan of the Foundation for Delaware County. That’s a significant burden for a system with $660 million in revenue in 2021 at its two major hospitals, according to filings with the Pennsylvania Health Care Cost Containment Council. To put that $35 million in perspective, it is more than enough to pay the annual salaries of the 215 people laid off this month.
Prospect Medical has stopped making those payments. In its annual report, Medical Properties Trust, the new owner, which is publicly traded and must report financial data to the Securities and Exchange Commission, revealed it has written off $283 million in losses for bad debt real estate, including $171 million for the Pennsylvania properties rented by Crozer.
Those high rent payments may have been why non-profit ChristianaCare, in Wilmington, Delaware, last year walked away from negotiations to buy Crozer Health from Prospect Medical, which is now trying to unload the system. A spokesperson for ChristianaCare refused to comment. “We hope they will sweeten the deal for another buyer to walk back in,” said Sheehan of the Foundation for Delaware County. “I don’t think they’ve sweetened it enough.”
Those hoping to spare their safety net hospitals from the predatory practices of private equity and other financial firms should look at Rhode Island. In the nation’s smallest state, where Prospect Medical and the privately held Steward Health Care (backed by the private equity firm Cerberus Capital Management) also operate, a law passed in 1997 gave Rhode Island’s attorney general and health department veto power over hospital acquisitions.
“When Leonard Green tried to sell its stake in Prospect, the attorney general in Rhode Island required them to set up an escrow to make sure pensions were paid,” said Sam Arnold, a legislative aide to Tim Kearney, the Pennsylvania state senator who represents half of Delaware County. Senator Kearney is preparing legislation to give the state’s attorney general and health department similar authority. Arnold told me that Leonard Green “needed to have skin in the game since they were leaving Prospect with this huge debt and no resources to pay for it.”
Kearney’s legislation allows state officials to challenge transactions that do not serve the public interest as well as stop recapitalizations and real estate sales “when it’s clear it will destabilize the finances of the health care system,” Arnold said. The goal is “to stop sales to irresponsible owners with track records of raiding hospitals.”
Of course, that won’t help Crozer, which is on the cusp of bankruptcy. Perhaps here, too, Pennsylvania and other states with hospital systems victimized by private equity may follow in the footsteps of Rhode Island.
In November, Prospect Medical agreed to sell its two major hospitals and six ancillary facilities in Rhode Island, known locally as CharterCARE Health Partners, to an Atlanta-based non-profit called The Centurion Foundation, organized in July 2021 to own and operate health care facilities. Prospect Medical’s Rhode Island operations were not included in the 2019 sale and leaseback arrangement that Leonard Green executed with Alabama-based Medical Properties Trust.
But Rhode Island officials reviewing the deal should scrutinize any new non-profit that suddenly appears on the scene and helps smooth a private equity deal. “Centurion focuses on reinvesting operating profit into its facilities, people, and communities it serves,” says the organizations’ joint press release issued by CharterCARE Health Partners and The Centurion Foundation. But its ability to do that will depend entirely on how much it pays Prospect Medical for the real estate, which will drive how much those facilities will pay in rent to retire the bonds Centurion must sell to buy the properties.
I called Centurion, which was launched just two years ago, to learn more about its founders. I wanted to know whether it had a conflict-of-interest-free relationship with Prospect Medical and Medical Properties Trust and whether it is negotiating with either company to execute a deal in Pennsylvania similar to the CharterCARE one in Rhode Island. The Centurion Foundation’s CEO, Greg Grove, a former investment banker, had a 30-year career at The Guardian Foundation, a non-profit with the mission of rescuing the flailing finances of nursing homes bought and flipped by private equity firms.
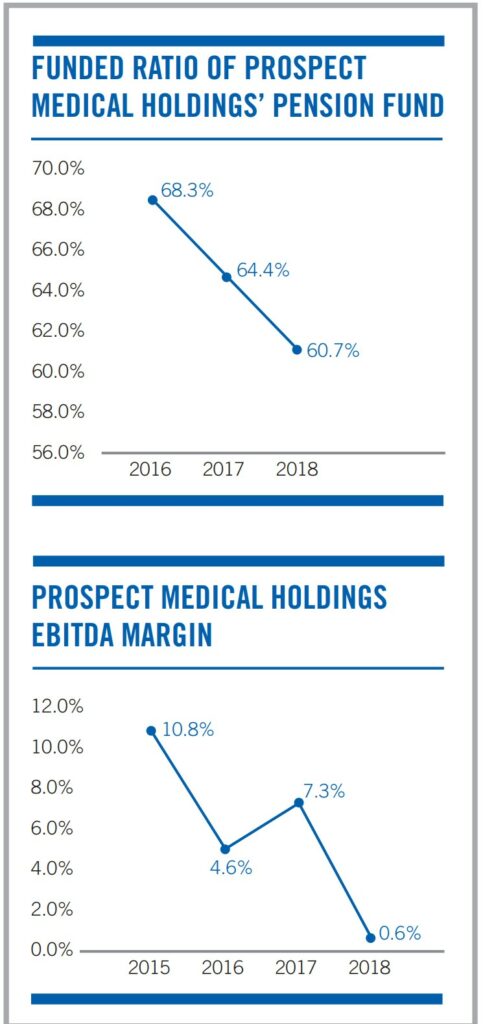
Leonard Green-led ownership collected $658 million in dividends and fees from Prospect Medical Holdings, pestakeholder.org. (Graphs and CharterCare).
Grove said he would put me in contact with someone with more knowledge about the situation. I was called a few hours later by Gary Hopkins of Blanco + Hopkins, the same P.R. firm that represents Prospect Medical. He said there would be no comment. Is it a coincidence that the same PR firm represents both The Centurion Foundation and Prospect Medical?
Fortunately, Rhode Island’s attorney general and health department will have the final say on whether the CharterCARE-Centurion Foundation deal is in the public interest. That’s how it should be when private equity funds and their hospital operator partners are eyeing their next target.