SCOTUS Rebuffs United Healthcare Medicare Advantage
This is an interesting result I ran across in MSN as taken from Reuters. Both Kip Sullivan and I have written about Medicare Advantage plans over coding patients, resulting in overcharges to CMS Medicare. “Why is CMS Overpaying United Healthcare Medicare Advantage Plans?” – Angry Bear, “Medicare Advantage and Medicare Issues” – Angry Bear, “Kip Sullivan and Ralph Nader Talk Tradition Medicare vs Medicare Advantage” – Angry Bear, etc. Advantage Plans code patients and then treat them. The plans receive payment for the coding before treatment. If United Healthcare Advantage over codes, they are paid. If the patient is not treated the Advantage Plan keeps the funds.
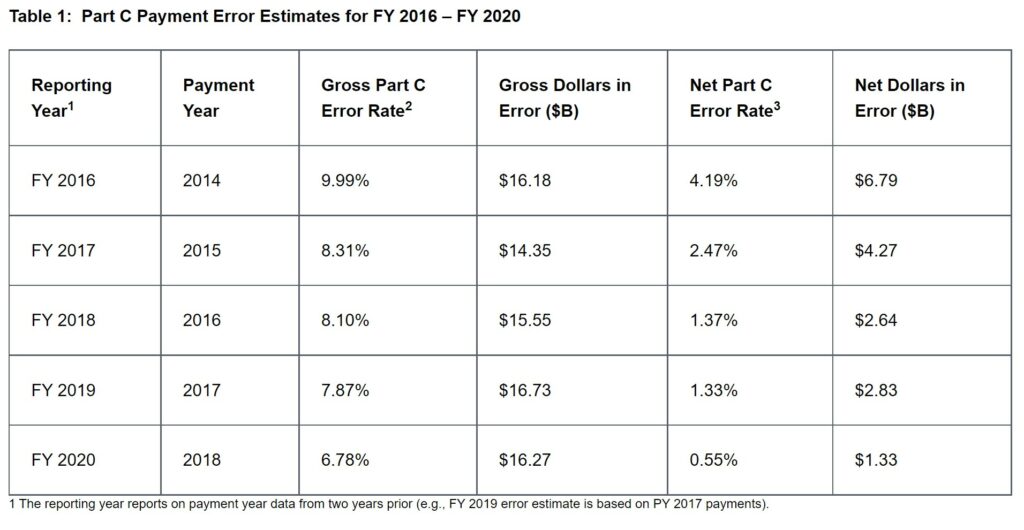
The chart covers years 2016 to 2020 reporting year for previous years 2014 to 2018.
“UPDATE 3-U.S. Supreme Court rebuffs UnitedHealth Group challenge on Medicare Advantage overpayments,” (msn.com), Brendan Pierson
UnitedHealthcare Insurance v. Becerra, 21-1140
June 21 (Reuters) – The U.S. Supreme Court on Tuesday declined to hear UnitedHealth Group Inc’s challenge to a government rule requiring private insurers that administer federally funded Medicare plans to return potentially billions of dollars in overpayments they receive based on incorrect diagnoses.
Turning away the Minnetonka, Minnesota-based insurer’s appeal, the justices left in place a lower court’s decision reviving the rule after a federal judge had previously struck it down.
UnitedHealth said in a statement that it would continue to comply with federal rules and “remain focused on providing high quality and affordable healthcare to millions of seniors.”
The 2014 rule applies to Medicare Advantage insurance plans, which are funded through the Health and Human Services (HHS). They are administered by private insurers like United Health. HHS pays Medicare Advantage plans a base amount per beneficiary, adjusted according to diagnostic codes reflecting each beneficiary’s individual risk factors.
Under the rule, if a Medicare Advantage insurer becomes aware of it receiving a payment based on an unsupported diagnosis, it must return that payment within 60 days. According to a 2016 federal audit, the government paid out about $16.2 billion that year based on unsupported diagnoses, nearly 10% of the total paid to Medicare Advantage insurers.
This has been going on for a number of years. “Medicare Advantage and Medicare Issues” – Angry Bear See chart above for years 2016 – 2020.

I like how Medicare Advantage is about creating market efficiencies, and UHC is definitely improving their margins with theirs.
once upon a time i thought single payer could get around the “market efficiency” dodge by contracting out insurance contracts the way the highway division contracts out the actual work. but the highway div sets the standards and inspects the project daily.
it is possible insurance contractors could discover the efficiencies and require the providers to follow them. on the other hand, as an arrogant sob myself, i would not like someone telling me how to do my work. on the other hand, the payor could say, “fine, do it your way. but we will pay for it our way.”
but you’d think something like this would happen anyway with the government setting the standards and prices, and closely inspecting the work. i don’t have great faith in “market efficiencies”…as compared to “goverment waste.’ government does a very different job than private sector. but as between government graft and private sector graft…. well, what i think works bsst is private sector competition to get the contract, and public sector inspection to discover the graft and look for efficiencies along side the contractor.
but, like i was getting to say, i can’t imagine why this isn’t happening already.
typo inspection report
faith not face