Medicare Could Use the VA’s Negotiation Results on Insulins and Other Drugs
VA-Like Negotiations on Insulin Prices Could Save Medicare Billions, MedPage Today, Zeena Nackerdien, February 21, 2020
I am going to dispense with the reasoning dissing the increased pricing of Insulin and go straight to a pricing strategy. Suffice it to say, the various versions developed of Insulin do not justify the pricing increases seen today.
Recently, Philip Longman (“Best Care Anywhere”) was advocating for Medicare pricing for everyone using commercial healthcare insurance. The only problem with this approach is we are not getting to the root cause of increasing prices for pharma, hospital supplies, and hospitals. Kocher and Berwick breached the same topic with their plan to transition from today’s Commercial Healthcare Insurance to Single Payer by reducing insurance premium growth rates – “limit hospital prices to Medicare prices plus 20 percent.” The authors of this particular article (originally in JAMA) on Medicare advocate using VA Pricing for Insulin. Further down is a second article taken from JAMA Network (which I have access to) advocating the use of VA pricing for orally-taken drugs also ands using an approved formulary.
Talking about VA pricing for pharmacy after the leap.
While government agencies in many countries negotiate prices directly with pharmaceutical companies helping to drive down the costs of medicines, the U.S. has long adopted a free market attitude towards prescription drugs as well as other commercial products. Drug companies through PBMs negotiate costs and pricing with private insurance companies nationally to secure the best tier possible. Historically the largest buyer of drugs has been blocked by Congress to negotiate drug prices which leaves Medicare at a disadvantage.
On the other hand, the VA receives a prescription drug discount, negotiates pricing, and creates a formulary to limit outpatient drug spending. In a JAMA Internal Medicine Research Letter, William Feldman, MD, of Brigham and Women’s Hospital in Boston, and colleagues reported that if Medicare Part D negotiated drug prices like the VA and used the same formulary, the government could have saved up to $4.4 billion on insulin costs in 2017. I do not have access to the complete version of this letter other than a brief JAMA Editorial Content paragraph.
The US Department of Veterans Affairs (VA), unlike Medicare Part D, receives a minimum discount for prescription drug purchases and additionally relies on price negotiation and a national formulary to limit outpatient drug spending. A 2019 study found that Medicare could have saved $14.4 billion in 2016 from an estimated $32.5 billion in spending if it used VA-negotiated prices for the 50 costliest Part D oral drugs. Inhaled and injectable products represented 16 of the 50 costliest drugs covered under Medicare Part D in 2016. Recently, our research group reported that Medicare could have saved $4.2 billion of an estimated $7.3 billion in spending on inhalers in 2017 by using VA-negotiated prices and the VA formulary.
Reviewing the 2017 Medicare Part D Drug Spending Dashboard, the Historical VA Pharmaceutical Price Files (obtain 2017 prices), and the 2019 VA National Formulary (with recent formulary changes) to compare insulin prices for Medicare Part D and for the VA, Feldman and team looked at 31 different insulin products across six classes.
Medicare receives rebates from drug companies to which the researchers estimated to be a 41% rebate in 2017 and which was based on data from the U.S. Government Accountability Office. This meant that the pre-rebate insulin costs of $13.3 billion dropped to $7.8 billion on the insulin products under investigation.
If Medicare used VA-negotiated prices, Medicare Part D spending would have decreased $2.9 billion more to $5 billion — a greater savings versus after rebates. Implementing the VA’s formulary restrictions within each insulin class (and used national contract prices), the estimated total Part D spending would have decreased further to $3.5 billion. Feldman and his team estimated a saving of $4.4 billion after post-rebate spending.
In a sensitivity analysis, Feldman and team showed that even if the assumed Medicare rebates were higher, savings associated with use of VA-negotiated prices and the VA formulary would have been $1.1 billion.
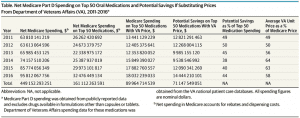
Rebate information from companies is confidential the same as negotiated pricing is confidential between countries which the World Health Organization has complained about in their paper on Cancer Drug Pricing. I do not have access to JAMA Internal Medicine; but, I can get into JAMA Network and there is a similar study there plus their Research Letter. “Assessment of Spending in Medicare Part D If Medication Prices From the Department of Veterans Affairs Were Used,” Brett Venker, Pharm; Kevin B. Stephenson, MD; Walid F. Gellad, MD, MPH, January 2019. This Research letter has a similar chart I am sure exists in the Feldman study. The Venker, Stephenson, and Gellad Research Letter reports on findings gross spending, spending using Medicare rebates, Medicare spending using VA pricing, and savings from using VA pricing. then on the top 50 oral drugs.
I made this chart large so it is easier to read and evaluate what can be saved if VA pricing was used for Medicare along with Medicare rebates. JAMA Internal Medicine editor at large Robert Steinbrook, MD, noted that the researchers’ estimates (Feldman Study) could be imprecise; but he said he supports the conclusions. “Even if the $4.4 billion figure overestimates the potential savings, the potential for lower prices would substantially increase many patients’ access to life-saving insulin products.” That savings and pricing results are on Insulin alone.
The chart shows oral drugs. For 2016 using VA pricing for the top do drugs, there is a potential savings of greater than $14 billion. We are just talking Medicare.
Steinbrook: the study by Feldman’s group is one in a series that the journal has published recently to show how $billions could be saved annually by the Medicare Part D prescription drug program.
“These studies have a consistent and clear message,” Steinbrook wrote. “At present, the issue for the federal government is not the ability to easily save billions of dollars each year in Medicare Part D spending. Rather, the issue is the political will in Washington, D.C., to facilitate savings through legislation and regulatory changes, such as measures that would allow price negotiations, benchmark pricing, and formulary restrictions, and in states to remove prescribing barriers, such as those for generic substitution and therapeutic interchange.”
The plan should include savings and pricing for all and not just Medicare recipients. It should be applied to more than just drugs.

This probably fits an earlier post called “Bargaining power, progressive maximalism, and Medicare for All” but that discussion seems to have stalled so I am posting the info in a comment here.
In the earlier post Erik Kramer was discussing the idea that if Pharma prices are reduced too much in a Single Payer Healthcare system then Pharma will not have the money to innovate new drugs. I made some counterpoints to his view and the comment in Stoller’s blog below seems to reinforce my argument that many Pharma drug prices are inflated due to greed and not due to the expense of R&D innovation.
This was a comment in this post in the blog BIG by Matt Stoller:
https://mattstoller.substack.com/p/the-coronavirus-crash-a-merger-boom
From the link related to the Pharma price discussion:
I got this great note from Yale economics professor Florian Ederer on innovation.
Although we disagree on many issues related to antitrust, I am an avid reader of your newsletter. Yes, I am an economist, but we’re not all bad…
The idea that large incumbents don’t want to innovate because such innovation would threaten their own cash cows goes back all the way to Kenneth Arrow (an economist that you would have liked) in the 1960s.
In our “Killer Acquisitions” paper we document the same effect in pharmaceuticals where dominant incumbents acquire small entrepreneurial startups and then kill the innovation because it would otherwise cannibalize the profits of their own existing drugs: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3241707
There are also other papers that show that increasing concentration is terrible for innovation in pharma (https://econpapers.repec.org/article/eeeindorg/v_3a63_3ay_3a2019_3ai_3ac_3ap_3a283-325.htm): horizontal mergers not only decrease the innovation intensity of the merging parties, but even the incentive to innovate of other competitors.
best,
Florian Ederer
Associate Professor of Economics
Yale University, School of Management
Jerry (Florian):
I am surprised Barkley did not answer you. Both Eric and Barkley are economists I think they both (Barkley does) teach also. Peter Dorman is a teaching economist as well as PGL. Robert Waldman teaches at the University of Rome. Me?
I am not a Doctorate like they are and stopped at my Masters out of Loyola University – Chicago. Tassos Malliaris was my Prof and we still talk now and then. I sometimes go and talk to his 4th year students on how not to be an ugly American in their Asian travels. I believe Tassos had hopes I would continue on to Chicago for my Doctorate. With 2 at home and a 3rd on the way I changed course in my thirties. Do I regret it? I think about it sometimes and just keep moving onward.
I once talked to Matt about writing here also. He went a different way and chose to write at another good blog. He is wrong on supply chains out of China. By boat out of Shantou, Tianjin, Hong Kong, etc. they go to one of the west coast harbors (Long Beach, LA, Portland, etc.). They can even go to Texas or Alabama. With the canal being able to allow larger ships, they can get to the east coast now and cut out rail. Once on the west coast, the container ships (or ro-ros) are unloaded and loaded on to flatbeds to make the journey. Figure three weeks on the water (some ships go faster now), one week in customs and port, and one week by train to Chicago to be switched to another train. This is the automotive route. I am a supply chain and manufacturing planning guy.
It is interesting, Congress dropped the 10 year exclusivity out of the NAFTA bill only to have the House put a 12 year exclusivity bill in the House Budget bill for Biologics and similar.
That opens the door for what I will bring up next; “TECHNICAL REPORT Pricing of cancer medicines and its impacts.” Start at page 13 and read to page 31. All the information is there on:
Industry’s pricing approaches, Relationship between inputs throughout value chain and price setting, Costs of production, Determining the value of medicines, Achieving income expectation, Financial returns to incentivize investment in R&D, Market structure for cancer medicines, Sources of market dominance, Pricing strategies of a monopolist.
Rather than buy them up, they also pay them not to produce. Or you can do like Mylan did with Teva and what they said was a generic version of the EpiPen. Mylan wrote a letter to the FDA stating since the Teva pen could not be used by following the EpiPen instructions, it is not a generic version. It is all about rent – taking. EpiPen changed the product to get an extension of exclusivity.
I know Eric does not believe we can cut into their pricing too much as they will lose momentum (not enough cash) to do R&D The ICER does a lot of the pricing for the drug industry. The did price Novartis Kymriah at $1 million per does. Novartis chose $400,000 per dose instead. Even this price will be played out with the PBMs, rebates, and insurance paying the manufacturer directly or through someone else. The ICER did do a study on the increases in pricing of drugs over a 2 year period.
The ICER:
This can be found here: “Unsupported Price Increase Report – 2019 Assessment.” there are a few other links there also.
Bill
If this is too long to ? I will give you the short version, the price increases in healthcare are mostly unjustifiable whether looking at surprise billing, hospital in and out patient treatments, pharma, healthcare supplies, etc. I would stop at doctors – mostly.
Jerry:
Have you read the latest JAMA abstracts and articles on drug pricing?
Run, I would not stop looking at Doctors for pricing discussions. A la Arrow, it is fully agreed that doctor-necessitated health care services do not reside in a classical market as the consumer is insufficiently empowered far from being an ideal consumer in an open market. This type service, at the point of service, is plainly not a place to expect market like forces to be working.
But there is well known incentives for doctors to use this unmarked like situation and we see this in practice norms that foster more utilization (see Wennberg stuff and Cochran stuff) while unit pricing and aggregates of top line revenues for doctor and dentist practices continue to rise.
It is also well known that a large number of persons in the highest income strata are doctors. This also begs for economics and policy analyses, inviting a very strong look at pricing.
And note how the point of service defines the cost structure for the intermediation structures that have layered themselves into this market less space or rude along with it, like the med-therapy pharma segment, ensuring that costs continue to rise for society.
Look at pricing at all parts of this place where market forces do not and can not work much at all. Decades of misaligned incentives are clearly viewable.
And look at the health outcomes, which can be improved.
Look at doctor and dentist pricing too.
Good Morning JF:
You are correct on Doctor salaries; however, they are less of the cause of today’s inflationary price increases without reason for them than the over prescribing of tests and meds. They do have some responsibility for it. I wrote this: “Another Look at Drug Pricing, Costs, and Why.” It has a comment on increases in doctor’s costs as made by a Commonwealth funded Health Affairs report in the txt of the post supported by a link to the report. There are some great links there and I hope you look at them also.
Run, thanks for the comment back. I am probably more concerned looking back over decades of misaligned economics in a non-market space. I have a memory, it is not people in our society who should pay for this policy neglect, in my view.
I look at a person who chooses to be a doctor instead of going into business. A business person is taking a risk and hopefully their subsequent efforts give them pricing room to be happy in their returns for the risk they are taking. Doctors face little risk with little hard capital needed (dentists more as they are equipment and technology-risk vulnerable more, IMO) and they have total control over the point of service. Business people would love to enter this space – little capital needed for entry, rising demand you do not have to market to much, total control over utilization and huge control over unit pricing, with a plain knowledge that these all rise in your favor. Who are we kidding. Most people do not want to be doctors and many can not become doctors, but who would object to this almost economically risk less business as a place to go for a livelihood; but I can be sorry for the statistics of decades telling me we can and should focus on pricing.
And we should do public welfare spending of huge amount to increase the number of doctors and other clinicians and free-up the work rules that apply too (and physical distributions).
I am ok with doctors making a whole lot less income going forward.
And honor them for their service while this regime is effected and supply helps bring some market like forces to work more on their income expectation.
JF:
So, we should ignore Commercial Healthcare insurance business, hospital and clinical business, Baxter, Abbott, Hollister, J&J, and other similar business, and concentrate on doctor salaries because you feel they have little risk in pursuing their trade?
I spent the last 10 or so years examining the healthcare issue, and yes doctors do play a part in the scheme of promoting more use of it when it results in over treatment, waste, and excess expenditures. Humira is the #1 drug sold in the US (outside of illicit opioids [which is another story]). I mentioned the ICER’s investigation of 100 drugs of which 77 had dbl digit price increases exceeding twice Medical CPI (if I recall this correctly). Of the nine chosen to be examined, 2 were dropped because they had shown data supporting their price increase could be associated with added value to society, the patient, healthcare, etc., and the seven remaining drugs no such legitimate detail to be taken into consideration.
Over and above what a doctor does, I believe the business of healthcare is a far bigger threat to us than how doctors practice medicine which in the end will be corrected. This is a comment by J & J CEO Gorsky:
If that last line not a thinly veiled threat, I am not sure what is. This is the attitude of the risk-taking-business has skin in the game and is more than adequately compensated as the Unsupported Price Increase Report which Institute for Clinical and Economic Review depicts; the Technical Report, Pricing of cancer medicines and its impacts which the World Health Organization depicts; the Trends in Prices of Popular Brand-Name Prescription Drugs in the United States, JAMA Network Open depicts; the Hospital Prices Grew Substantially Faster Than Physician Prices For Hospital-Based Care In 2007–14 which Health Affairs depicts; and Kocher and Berwicks’s While Considering Medicare For All: Policies For Making Health Care In The United States Better, Health Affairs.
Is it possible to ignore a 42% increase between 2007 -2014 for in patient care, a 25% increase in out patient care over the same period, and a 7% increase in doctor’s cost within the same hospital. Side note, 3rd party billing of a doctor’s care in patient or ER favors hospitals. This is big business rent taking because they can do it with a captive audience due to consolidation as ACOs. Even the AMA at ~20% membership does not have that power. We need to fix the business of healthcare first doctoring will follow. Kocher and Berwick called for payment rates for hospitals including doctors of 125% Medicare until single payer takes hold.
I have malfunctioning USB ports on my computer so it has a tendency to miss letters or numbers. Sorry!
Didn’t mean to imply that we should concentrate only on doctors. Just don’t want them excluded in the analyses, narratives, and change in the regimes that enable better healthcare delivery at lower costs to society.
If we had our way of enabling a better healthcare delivery system the very distorted flows that burden the society and its economics would find more useful purposes.
A single payer enablement would have incredible benefits for society compared to what we have now.
Enjoyed the discussion.
Thanks.
JF:
There is every intention for them to be included. They have to be. I think we should start with the big fish first and get to them eventually. Perhaps I did not say it yet; but, Single Payer will be down the road and we have to transition to it over time. I enjoyed talking to you also. Don’t be afraid to engage again. You are welcome here.
Bill
JF:
I have a post up on household humidity being used to minimize fomites in the air which are thought to ca the virus. I am curious as to your opinion on the Coronavirus near-epidemic (soon-to-be) in the US. Feel free to post your comment here. http://angrybearblog.com/2020/03/turn-up-the-humidity-in-your-house.html