Healthcare News
 Massachusetts ACA Enrollment Exceeds Last Year, Charles Gaba, ACA Signups Blog
Massachusetts ACA Enrollment Exceeds Last Year, Charles Gaba, ACA Signups Blog
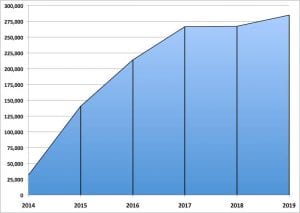
Massachusetts: (January 14, 2018) saw an increased 285,000 signups for healthcare for 2019 which is up 6.6% YOY and with 9 days left until the ACA signup deadline. This comes even though Republicans and Trump have been sabotaging the ACA. Even more impressive, 97.2% (90% National Average) of enrollees have paid their 1st month fees.
Republicans and Trump Implement the CSR again, Ban Silver Loading, and then Kill the CSR in 2021, Andrew Sprung, xpostfactoid blog
The Trump administration has called for an appropriation to fund CSR the old way — by reimbursing insurers directly for providing it. This comes after President Trump revoked the CSR subsidy used to help pay for deductibles, copayments, and coinsurance. When the CSR was revoked, ACA companies loaded the costs solely into the Silver plans in which they were used and resulted in Bronze and Gold plans to become less costly. Income-based ACA premium subsidies are based on a silver benchmark and silver loading generated major discounts in bronze and gold plans.
“For the first half of 2018: 16% percent of enrollees were enrolled in a plan with zero premiums after application of advance payments of the premium tax credit, 19 percent of enrollees paid a premium of less than 5 percent of the total plan premium.” This is largely the result of Silver plan loading, which created $0 premium bronze plans widely available and less costly gold plans which doubled in enrollments in 2018. There was also an increased enrollment of approximately 300,000 enrollees in 2018 with the likelihood of a 2-3 million boost in subsequent years.
So what is the issue? CMS released the annual Notice of Benefit and Payment Parameters (NBPP) January 17th. In its efforts to kill the ACA, CMS is calling for an elimination of Silver loading in 2021. Given the lowered cost of various plans resulting from Silver loading, Democrats should not be willing to sacrifice the silver loading windfall without trading it for a less haphazard boost to marketplace funding.
As xpostfactoid blog suggests, perhaps a cap on premiums as a percentage of income for all enrollees up to 600% FPL and improved subsidies for the 200 – 400%FPL.
Healthcare Job Growth Outpaces Nearly Every Sector in 2018, MedPage Today, John Commins
For 2018, healthcare created a total of 346,000 jobs or nearly 29,000 new jobs each month which is up from 284,000 jobs created in 2017. The 2018 figure includes 219,000 new jobs in ambulatory services and 107,000 new hospital jobs.
Healthcare job growth outpaced nearly every other major sector of the economy in 2018, including food services (261,000), construction (280,000), manufacturing (284,000), and retail sales (92,000).
The new data is in line with Bureau of Labor Statistics projections that healthcare sector employment will grow 18% from 2016 to 2026, much faster than the average for all occupations, adding about 2.4 million new jobs.
The VA’s Choice Program Meant to Eventually Replace the VA Gave Companies Billions and Vets Longer Waits, Isaac Arnsdorf & Jon Greenberg, Politifact
As a short-term response to a crisis, the VA paid contractors at least $295 every time it authorized private care for a veteran. The fee was high because the VA hurriedly launched the Choice Program to meet a ninety-day deadline from Congress in response to an Arizona VA facility not responding quick enough to veteran’s needs for healthcare and resulting in deaths.
Four years later, the fee never subsided — it went up to as much as $318 per referral.
Since 2014, 1.9 million former service members have received private medical care through Choice. It was supposed to give veterans a way around long wait times in the VA or travel long distances to be seen. But their average waits using the Choice Program were still longer than allowed by law, according to examinations by the VA inspector general and the Government Accountability Office. The watchdogs also found widespread blunders, such as booking a veteran in Idaho with a doctor in New York and telling a Florida veteran to see a specialist in California. Once, the VA referred a veteran to the Choice Program to see a urologist, but instead he got an appointment with a neurologist.
While it was true officials at the Phoenix VA were covering up long wait times, the inspector general eventually concluded that no deaths were attributable to the delays. However, critics seized on this scandal to demand that veterans get access to private medical care. As a safety valve for veterans, the Choice program is an alternative provided the quality of outcomes is there. My own experience with the VA has not been bad nor did my appointments take months. On the other hand, there are times I end up at clinics or the ED when I can not see my PCD.
An IG of the Choice program found the VA overpaid by $140 million besides other issues with the program.
Access to VA Health Services Now Better Than Private Hospitals? Nicole Lou, MedPage Today
Researchers find some wait times generally improved since 2014.
In 2014, the average wait for a new VA appointment in primary care, dermatology, cardiology, or orthopedics was 22.5 days, compared with 18.7 days in private sector facilities (P=0.20). Although these wait times were statistically no different in general, there was a longer wait for an orthopedics appointment in the VA that year (23.9 days vs 9.9 days for private sector.
The study, published in JAMA Network Open, found that wait times in 2017 favored VA medical centers (17.7 days vs 29.8 days for private sector facilities). This was observed for primary care, dermatology, and cardiology appointments — but not orthopedics, which continued to produce appointment lags in the VA system (20.9 days vs 12.4 days), the authors stated.
As resources in the VA are increasingly diverted to purchase care in the community, it remains to be seen if access to healthcare services can be maintained while access in the private sector continues to deteriorate, adding that virtual care may be one way to improve access given the non-infinite supply of face-to-face appointments.”
Fee-for-Service Must Go Says Ex-Vermont Governor Howard Dean, Joyce Frieden, MedPage Today
Dean, an internist and former Democratic governor of Vermont: “Under the current system, you only make money if people get really sick. Every financial incentive we have in American healthcare is to spend as much as we possibly can.
“We’re not getting paid for keeping people healthy in our system. I don’t believe that doctors think it’s a wonderful idea to have people get sick. But incentives work in every system … and monetary incentives always work in human beings. If you keep the incentive system the way it is, you have a distorted system that works against good health.”
As for universal care in the U.S., I’m not necessarily opposed to Medicare for All, but the problem is it’s a fee-for-service system so we’d have to fix that. The only way you can really save money is with capitated care.”
by run75441 (Bill H)
