Small Town and Rural Hospitals Are at Risk of Closing due to Funding
This is an interesting take on small hospitals and also covering smaller hospitals in small towns or rural areas. It is an issue as the larger hospitals buy them up. Rather than invest in them, they close them down. One reveal is those hospitals closings coming as a result of what private insurance pays for patient care.
This is an issue which both state and federal governments. should be addressing.
Why are 600+ rural hospitals at risk of closing? advisory.com. Commentary taken from:
“Rural Hospitals at Risk of Closing,” chqpr.org. Center for Healthcare Quality and Payment Reform.
Things are changing more rapidly. Smaller hospitals are under an attack of high costs and less revenue. As a result, many are closing leaving the small town and rural residents without medical care or having to drive long distances in emergencies. As reported by Healthcare Quality and Payment Reform:
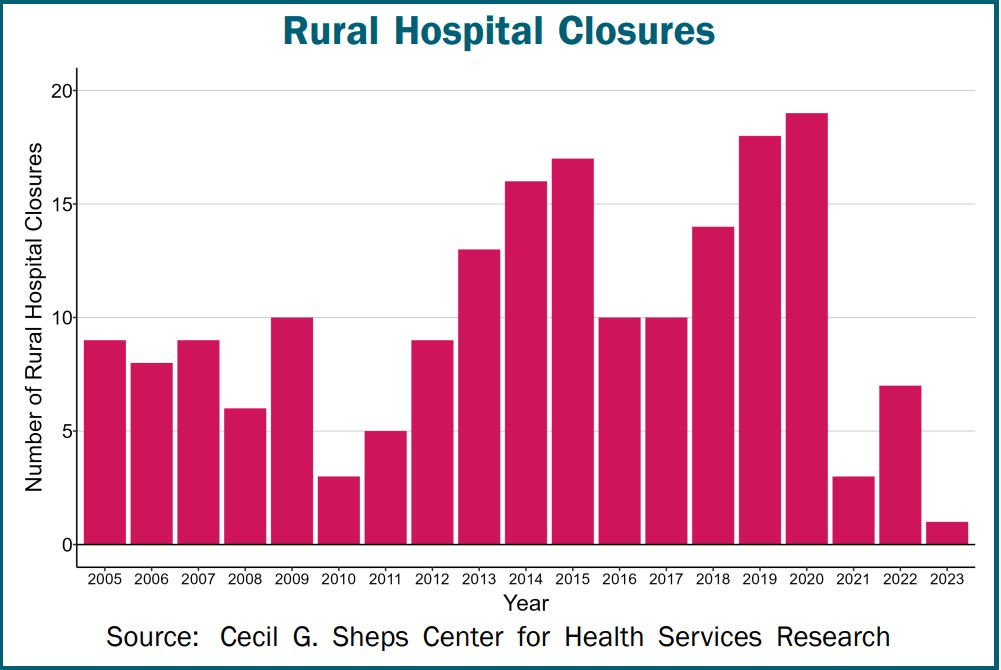
Many people across the country could not receive hospital care in their community when the pandemic began. Over 150 rural hospitals closed between 2005 and 2019. An additional 19 rural hospitals closed in 2020, more than any year in the previous decade. The closures are not resulting from the pandemic, but by financial losses in previous years. Ten more rural hospitals closed in 2021 and 2022. The closures decreased in 2019 due to the special financial assistance hospitals received during the pandemic. The pandemic aid has ended and closures are likely to increase.
Hundreds of Hospitals are at Risk of Closing
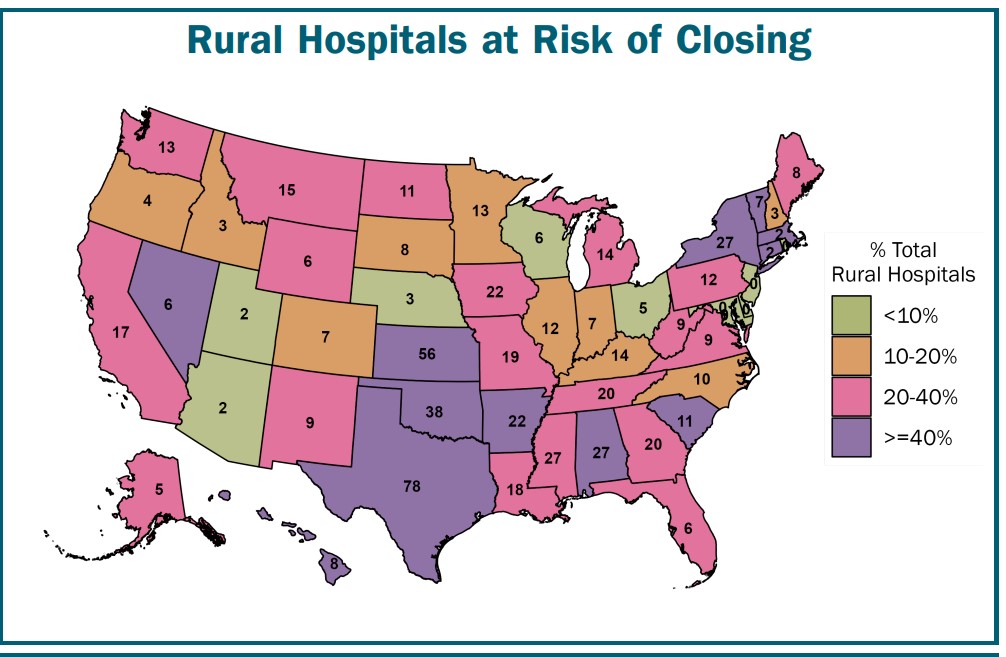
Six hundred rural hospitals or ~ 30% of all rural hospitals in the country are at risk of closing. At risk because of the serious financial problems, they are experiencing:
Losses on Patient Services: Health insurance plans are not paying these hospitals enough to cover the cost of delivering services to patients. The losses will likely be greater in the future due to the higher costs. All hospitals and particularly small rural hospitals are experiencing such because of inflation and workforce shortages. Many of these hospitals have received grants, local tax revenues, or profits from other activities offsetting losses on patient services in the past. However, there is usually no guarantee these funds will continue to be available in the future or whether they will be sufficient to cover costs.
Low Financial Reserves: If the hospitals do not receive grants or other funds to cover losses on services, the hospitals would not have sufficient net assets (including pandemic-related funding, but excluding buildings & equipment) to offset their losses for more than 6-7 years.
Many Rural Hospitals Are at Immediate Risk of Closing
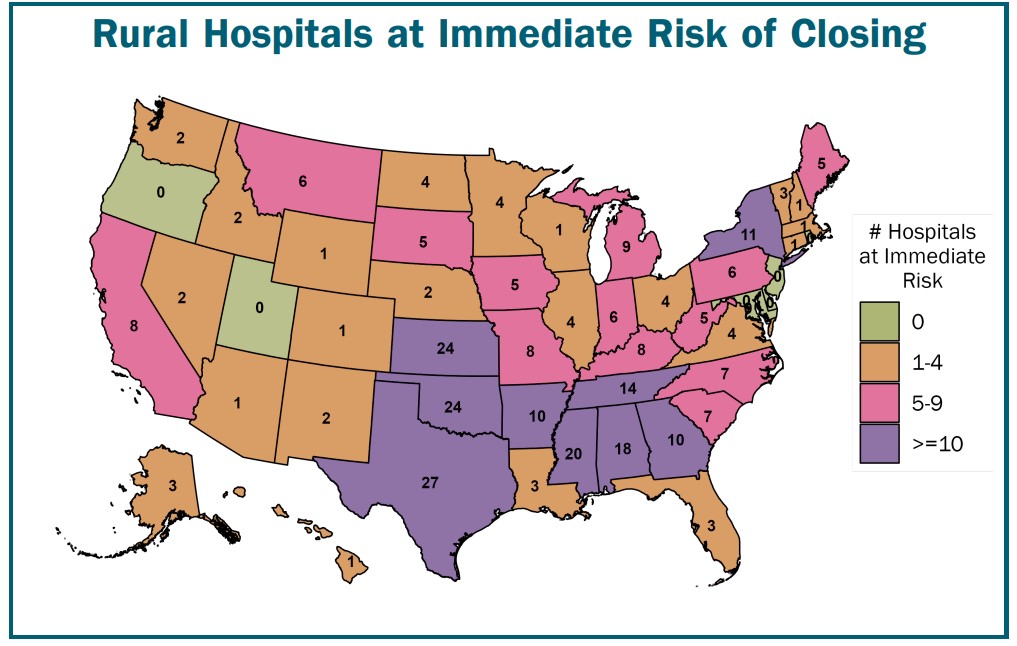
Over 200 of rural hospitals are at immediate risk of closure. This due to the severity of their financial problems:
Inadequate Revenues to Cover Expenses: These hospitals lost money delivering patient services over a multi-year period (excluding the first year of the pandemic). They are unlikely to receive sufficient funds from other sources to cover those losses after federal pandemic assistance ends.
Very Low Financial Reserves: The hospitals have more debts than assets, or the hospitals’ net assets (including pandemic-related funding and excluding buildings & equipment) could offset their losses for at an ~ 2-3 years. (Fewer rural hospitals are at immediate risk than prior to the pandemic because of the federal pandemic aid they received).
Access Reduction and increasing Disparities for Rural
Most of the at-risk hospitals are located in isolated rural communities. Closure of the hospital would mean residents of the community would ravel a long distance for emergency or inpatient care. Also in many small rural communities, the hospital is the only place where residents can get laboratory tests or imaging studies. It may be the only or principal source of primary care in the community. A closure of the hospital would cause a loss of access to many essential healthcare services.
What I like about this article is it adding a different viewpoint of why small hospitals are in financial trouble is the next portion of the article. The next two topics come as a shocker.
Closures Are Caused by Inadequate Payments from Private Payers
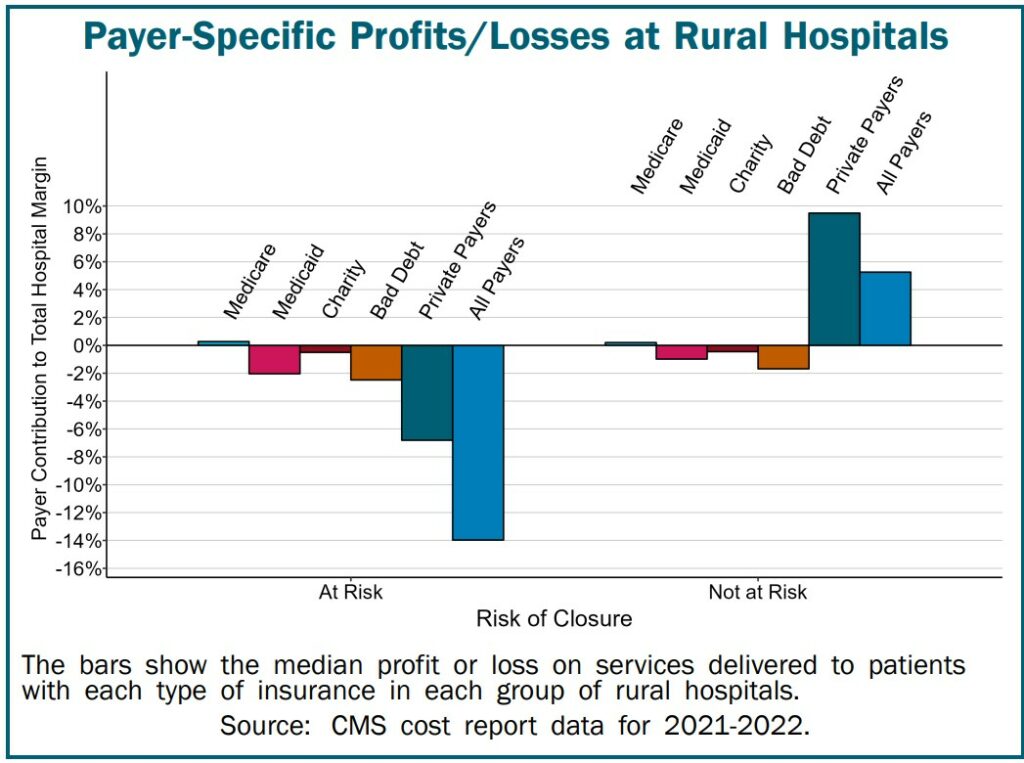
The primary reason hundreds of rural hospitals at risk of closing is private insurance plans are paying them less than what it costs to deliver services to patients. As shown, although the at-risk hospitals are losing money on uninsured patients and Medicaid patients . . . losses on private insurance patients are the biggest cause of their overall losses.
Conversely, many rural hospitals not at risk of closing because they make profits on patient services. They receive payments from private health plans covering the costs of delivering services to the patients with private insurance. Those payments also offset the hospitals’ losses on services delivered to uninsured and Medicaid patients.
Note: Medicare is not one of the causes putting rural or small hospitals at risk.
Preventing Rural Hospital Closures
Changes are being called for in both the amounts and method of payment for rural hospital services in order to prevent more rural hospitals from closing in the future. Rural hospital closures threaten the nation’s food supply and energy production. The reasoning are the locating of Farms, ranches, mines, drilling sites, wind farms, and solar energy facilities are located primarily in rural areas. They will not be able to attract and retain workers if the workers cannot get adequate healthcare services.
Requiring Healthcare Services to Cover the Cost of Services in Rural Communities
Payments that are sufficient to cover the cost of services at large hospitals will not be adequate at small rural hospitals because it costs more to deliver healthcare services in rural communities. This is not because rural hospitals are inefficient, but because of the smaller number of patients served relative to the fixed costs of the services. For example, a small rural community will have fewer Emergency Department (ED) visits than a larger community simply because there are fewer residents, but the minimum cost of staffing the ED on a 24/7 basis will be the same, so the average cost per visit will be higher.
The biggest problem facing small rural hospitals is inadequate payments from private health plans. Most “solutions” for rural hospitals have focused on increasing Medicare or Medicaid payments or expanding Medicaid eligibility due to a mistaken belief most rural patients are insured by Medicare and Medicaid or are uninsured.
In reality, about half of the services at the average rural hospital are delivered to patients with private insurance (employer-sponsored insurance and Medicare Advantage plans). In most cases, the amounts these private plans pay, not Medicare or Medicaid payments, determine whether a rural hospital will have to close.
Rural hospitals should not be forced to eliminate inpatient care in order to receive higher payments for other services, as is required under the federal “Rural Emergency Hospital” program. This would make it harder for rural residents, particularly the elderly, to receive prompt, high-quality care when they are ill.
Increasing payments to levels sufficient to prevent closures of the at-risk hospitals would cost about $4 billion per year. This would represent an increase of only 1/10 of 1% in total national healthcare spending. Most of the higher spending would support primary care and emergency care, since the biggest causes of losses at most small rural hospitals are underpayments for primary care and emergency services. Spending would likely increase as much or more than this if hospitals close, because reduced access to preventive care and failure to receive prompt treatment will cause residents of the communities to be sicker and need more service in the future.
Create Standby Capacity Payments to Support the Fixed Costs of Essential Rural Services
The financial problems at small rural hospitals are caused not only by the inadequate amounts paid by private health insurance and Medicaid plans, but by the problematic method all payers use to pay for services. Small rural hospitals are not paid at all for what residents of a rural community would likely view as one of the most important services of all – the availability of physicians, nurses, and other staff to treat an injury or serious health problem quickly if the resident experiences an injury or problem. Having health insurance that pays fees for ED visits, laboratory tests, or treatments is of little value if there is no Emergency Department, laboratory, or treatment capability available in the community for the resident to use.
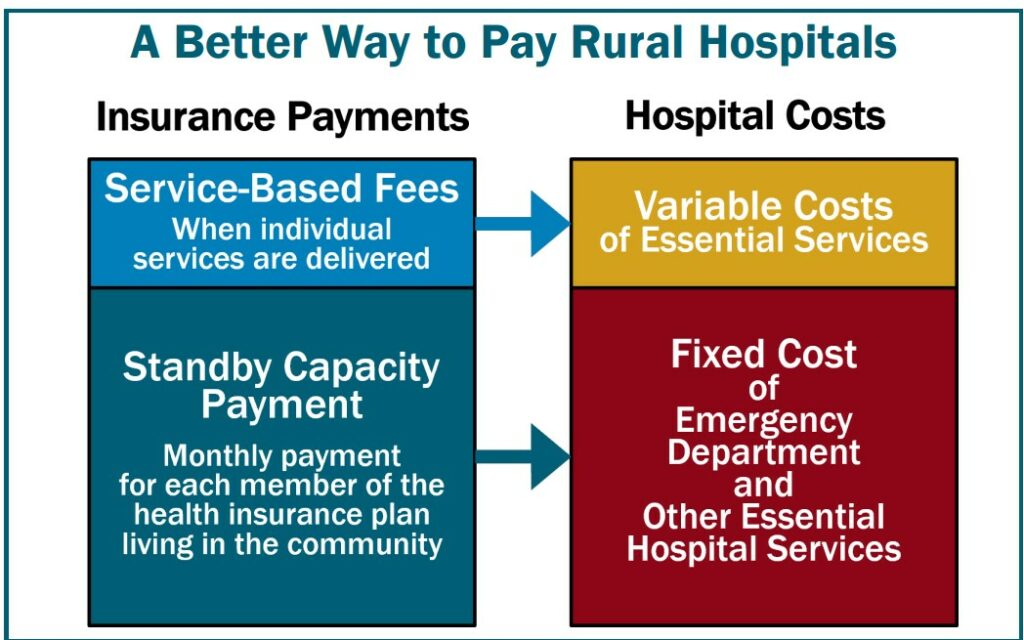
In order to preserve and strengthen essential hospital services in rural communities, small rural hospitals need to receive Standby Capacity Payments from both private and public payers in addition to being paid Service-Based Fees when individual services are delivered. The Standby Capacity Payment would support the fixed costs of essential services at the hospital, and the Service-Based Fees would cover the variable costs of those services.
More details on this approach are available in A Better Way to Fund Rural Hospitals.
Why Do Rural Hospitals Close? Angry Bear, angry bear blog

Charities lobbying to restore expanded tax deduction for giving
Temporary expansions meant to help charities stay afloat during the COVID-19 crisis expired at the end of the year
(The standard deduction that most people use now for their 1040’s means that people have no particular ‘tax incentive’ for charitable deductions, unless they still itemize, which is now uncommon.)