Cost of Rural Hospital Services
This is the start of a series of posts or commentary on access to hospitals in rural areas. First point, since they do not have the volume a hospital in the city has, their costs make be higher. The infrastructure and labor involved has to be spread over 24 hours of availability and not just when needed. In other words, you can not turn it on and off as needed. Availability to another source of care may be time limited depending on the patient too.
Second point is the cost of one service can be mitigated by the volume of other services. In other words, while the service may not pay for the cost of having it available, it can be covered by the overall availably of other services less costly and more revenue generating.
Ultimately, the costs may be higher for emergency department care in rural areas. Some of what they call overhead for such a department I would call Labor. If you have an Emergency Department, the costs are constant whether it is used or not. That is just one example. For this reason and to explain to readers, I am going to provide sections of this report on Angry Bear.
Cost of Rural Hospital Services – Saving Rural Hospitals by the Center for Healthcare Quality and Payment Reform (CHQPR)
Cost of Rural Hospital Services
Most Spending at small rural hospitals is for delivery of six essential services: (1) Emergency Department, (2) Inpatient services, (3) Laboratory, (4) Radiology, (5) Drugs and medical supplies, (6) and one or more Rural Health Clinics.
The impact of the costs of an Emergency Department is inherently higher at small rural hospitals than at larger hospitals. At least one physician needs to be available around the clock in order to respond to injuries and medical emergencies.
Costs of inpatient care, laboratory tests, imaging studies, primary care visits, and other essential services can be higher. For almost every type of service the hospital delivers, there is a minimum level of staffing and equipment required to deliver the service.
Fee-for-service payments increases the financial losses at small rural hospitals. The fee-for-service payment systems used by hospitals is the same no matter how many times the hospital delivers that service. Fewer services delivered and fee-for-service revenues decrease.
Eliminating inpatient care to prevent closure harms the hospitals and the communities. The revenues generated by inpatient care at a small rural hospital can exceed the direct costs of delivering care. The hospital would be worse off if it no longer received those revenues. Consider inpatient rehabilitation, and acute inpatient care. Loss of such deprives community residents of services and limits the ability of the hospital to respond to a pandemic, etc.
Major Categories of Expenses in Small Rural Hospitals
Direct Service Costs vs. Overhead Costs*
Most hospital expenses fall into two major categories:
- Direct Service Costs. Costs associated with personnel who provide the services individual patients receive, such as the nurses in the inpatient unit, the physicians and nurses in the emergency department, and the technicians in the laboratory.
- *Indirect Service Costs: Personnel who do not provide services directly to or for patients. The hospital’s accounting and billing departments, the human resources department, medical records, information systems, and maintenance. Non-patient service activities such as a gift shop, parking lot, or housing for staff.
- Overhead Costs: Costs of the equipment and supplies used to deliver services to patients. This also Includes the costs of building and maintaining the hospital’s infrastructure.
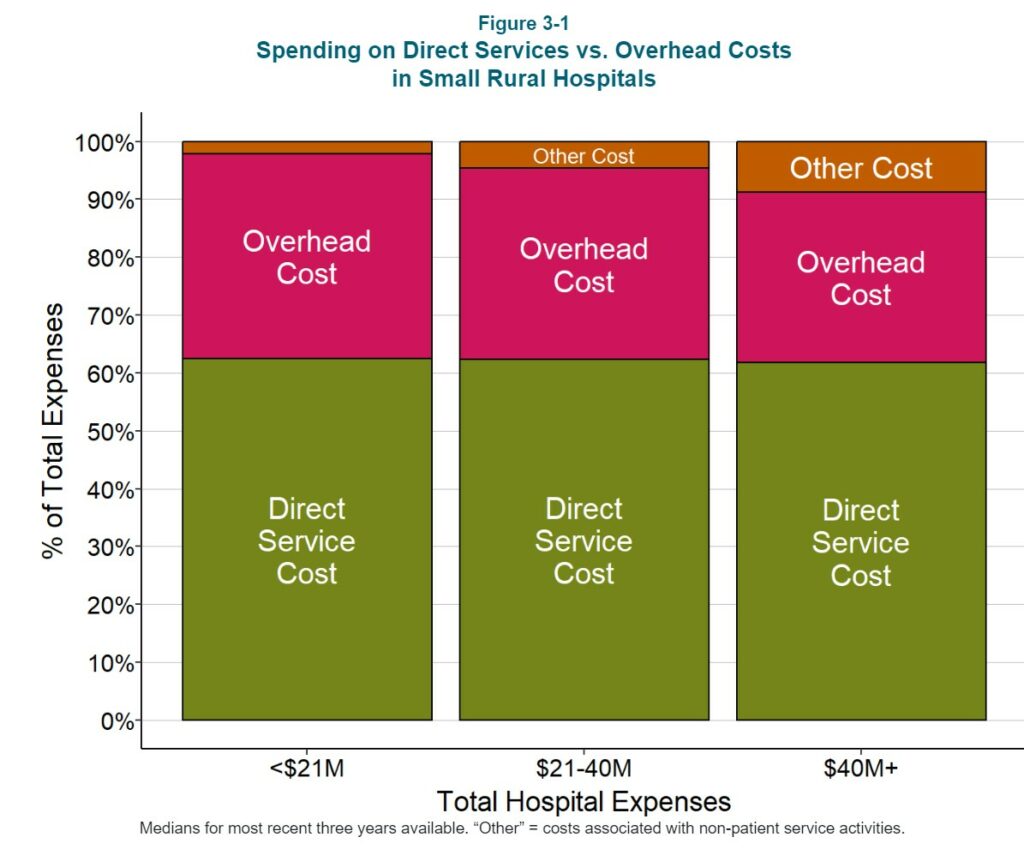
Approximately 60% of the total expenses of small rural hospitals is direct service costs, and ~35% consists of overhead costs. Non-patient service activities represent less than 5% of total expenses at most hospitals. *I broke this out differently than what the authors did. I added Indirect Service costs to include all Labor not directly involved with patient care. I also placed hospital equipment into Overhead costs. For now, I will use the author’s cost split.
The Largest Categories of Direct Service Costs
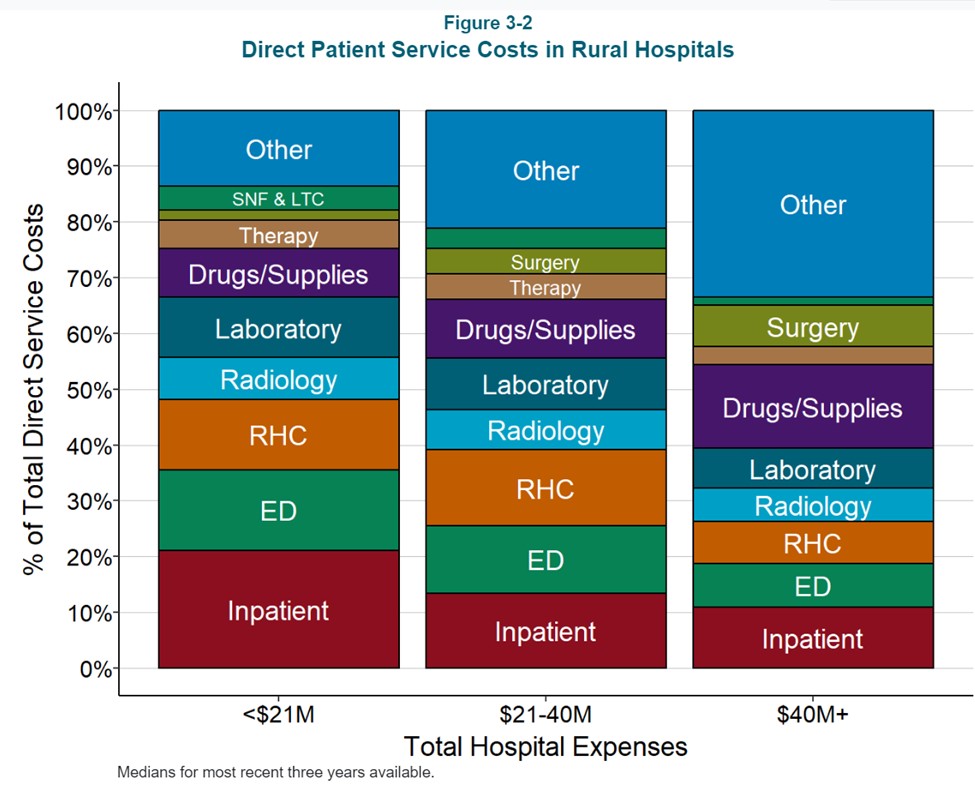
A core group of six services constitute the majority of direct patient service costs at small rural hospitals:
- the Emergency Department,
- inpatient services,
- the laboratory,
- radiology,
- drugs and medical supplies, and
- the Rural Health Clinic (if the hospital operates an RHC).
At small rural hospitals, these six core services represent over 60% of the hospital’s total direct patient service costs. Larger hospitals are more likely to offer other services, such as surgery and maternity care and to have larger numbers of patients receiving those services, so a smaller share of total costs at larger hospitals will be associated with the six core services, but the core services still represent more than half of direct patient service costs.
Categories of Overhead Costs
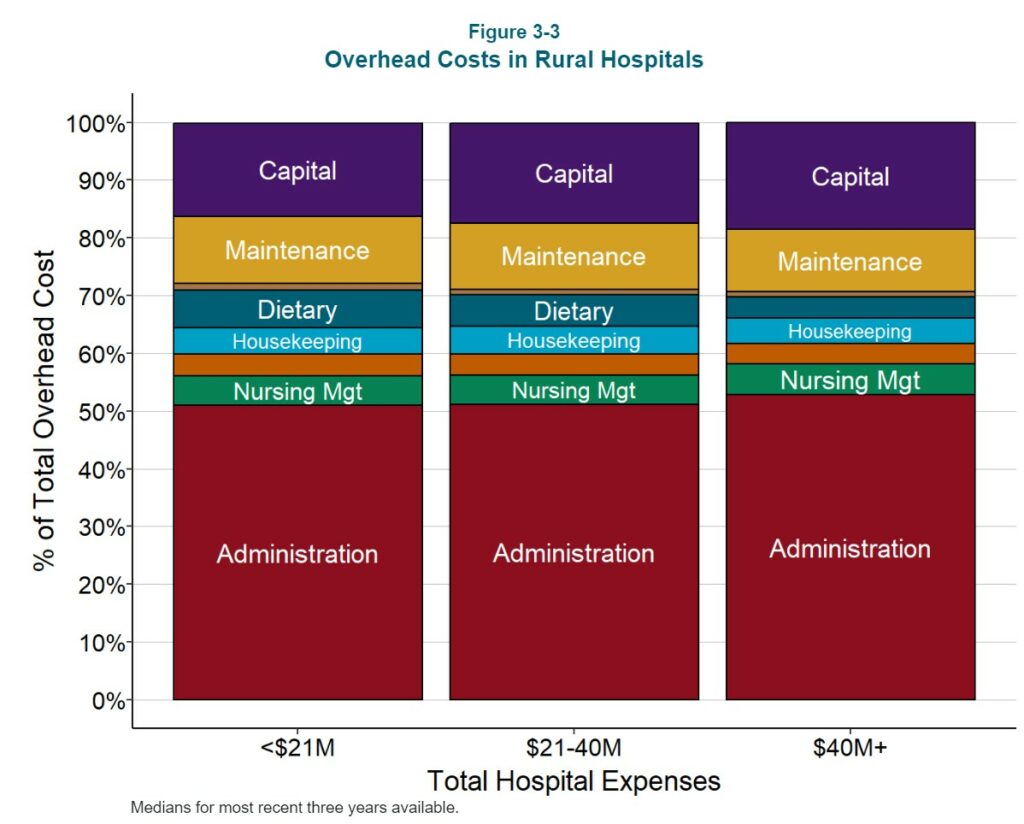
About half of overhead costs are for general administration of the hospital. This encompasses a broad range of activities, including accounting, human resources, billing, information systems, etc. Many small rural hospitals have had to spend large amounts of money to purchase and maintain an Electronic Health Record (EHR) system, and this contributes to the large share of costs in this category.
Not surprisingly, the second largest categories of costs are capital and maintenance costs, since it is expensive to build and maintain hospital facilities. On average, this represents nearly 30% of the total overhead costs at small hospitals.
The remaining 20% of overhead costs are associated with a variety of smaller functions, such as nursing management, medical records, housekeeping, dietary, and laundry services.
Since every hospital will need a minimum level of administrative services such as accounting, human resources, billing, etc. regardless of how many patients the hospital treats, one might expect that economies of scale would result in significantly lower administrative costs at the larger hospitals. However, the proportion of total expenses used for administrative costs is only slightly lower at larger hospitals.
Total Service Line Costs
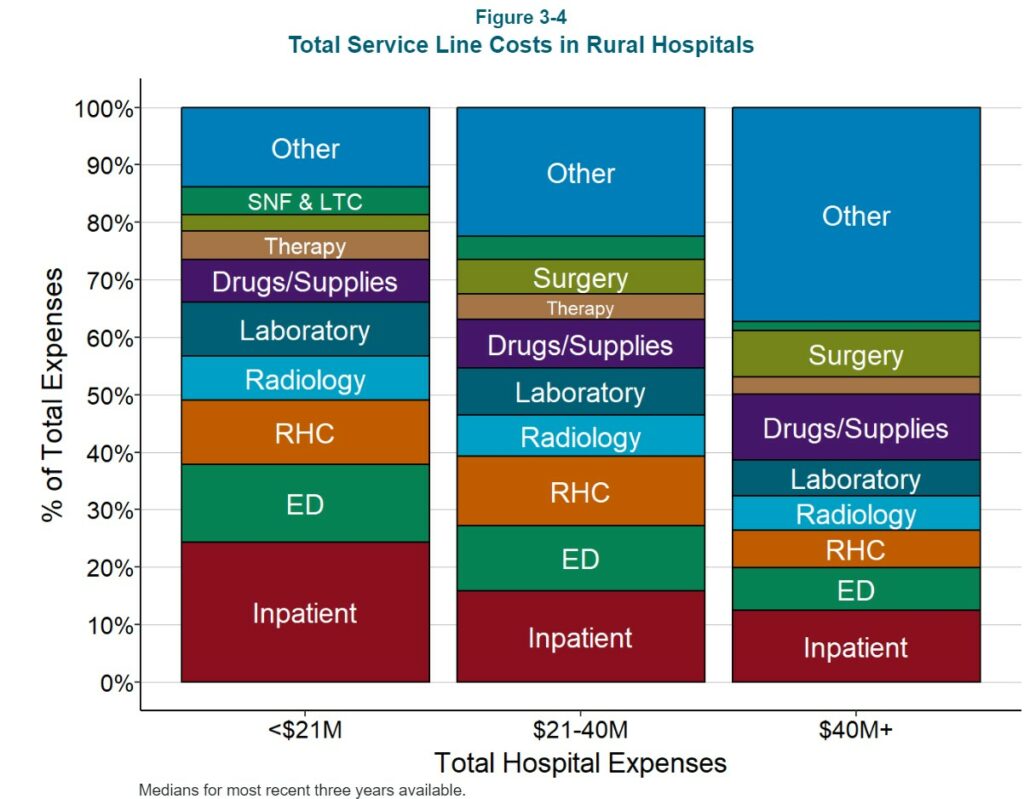
Hospitals are only paid for the services they provide to patients, so the payments the hospital receives for those services have to be adequate to cover not only the direct costs of the services, but also the overhead costs of the hospital. As a result, in order to set its charges for services, each hospital needs to allocate its overhead costs among the service lines.
The total cost of each service line will, on average, be about 60% higher than the direct costs when overhead costs are included. Since some services are more dependent on certain overhead cost centers than others, the percentages of overhead allocated to different service lines differ. For example, the inpatient unit is generally the largest user of the hospital’s dietary services, so a higher share of dietary costs is allocated to inpatient services.
Impact of Changes in the Number of Service Lines on Costs of Services
If a hospital is able to add an additional service line with little or no increase in administrative and overhead costs, the cost assigned to each of the existing service lines will decrease. This is because the hospital’s overhead costs are allocated across all of the hospital’s service lines, and so, all else being equal, the more service lines there are, the smaller the amount of overhead that will need to be allocated to each individual service line. As a result, the cost of a service line may differ at two hospitals not because of differences in the number of patients receiving the services, or differences in the staffing levels or wages paid to the staff, but because of how many other types of services each hospital offers.
An important corollary is that if a hospital eliminates a particular service line:
- The hospital’s total expenses will decrease by less than the total cost of the service line. Only a portion of the total cost allocated to the service line represents the direct costs of delivering that service. The rest represents a portion of the hospital’s general overhead expenses. It may be possible for the hospital to make some reductions in one or more central administration cost centers. However, when a service line is eliminated if the service line was a heavy user of those cost centers, in general, most of the hospital’s overhead costs will remain unchanged.
- The cost of every other service at the hospital will increase, because most of the overhead costs that had previously been allocated to the terminated service line now have to be recovered from the remaining service lines.
The Key Role of the Core Services on the Financial Viability of Small Rural Hospital
After allocation of overhead costs, the six core service categories still represent 60-70% of the total expenses at small rural hospitals. Because these services represent such a large proportion of the hospital’s total expenses, it will be difficult for a small hospital to be profitable if it does not receive payments for each of these core services. The payments must be adequate to cover the total (direct and overhead) costs of those service lines and if it cannot reduce the costs of the services to match the payments it is able to receive.
The Cost of Delivering Rural Emergency Department (ED) Services
The single most essential service rural hospitals provide is a 24/7 Emergency Department. Although emergency departments at small rural hospitals do not have the capability to treat severe trauma cases and emergencies requiring highly-specialized services, neither do many urban hospital EDs.
The primary roles all EDs perform are to quickly and accurately diagnose health problems, provide any necessary treatment to the patients, and transfer the small set of patients who need specialized care to a trauma center, stroke center, etc. Residents of rural communities not having access to an ED may be more likely to die or experience complications that could have been prevented.
The next section will examine the costs involved in operating Emergency Departments at small, rural hospitals. The focus in the section will be on the basic ED visit itself It will not include additional services a patient may receive during the visit that are delivered by other hospital departments, such as a laboratory test or an imaging study. The costs of delivering those other services will be examined separately below.
The next section will explore ED Visits to Rural Hospitals, Cost of Operating an ED With 10,000 Visits Per Year, Staffing, Direct and Indirect costs, and the Cost of Operating an ED with More or Fewer Visits Per Year.

Other rural hospital problems:
– The large number of uninsured patients. I know that hits our local hospital. There are fewer employers offering health insurance, and there are a lot of people just on the edge of the cash economy.
– The difficulty recruiting medical professionals. There is a salary premium for doctors and nurses, and, often, the only way to staff involves short term, higher priced contracts with individuals and medical staffing groups.
– The lack of human capital. Our local hospital is a non-profit with local, state and federal subsidies, but it is hard to recruit good managers. There are some good people on the board, but there is a limited pool.
Kaleberg.
All good points. Having Medicaid, Medicare, and VA sponsored payment covers much of the cost of the service. There is still a gap afterwards.
There is a tendency of short-term employees coming from medical employment agencies to be less involved. I clearly had a gall bladder issue and the idiot posing as a doctor claimed it to be indigestion and released me on a Friday. I returned on Monday to be hospitalized with an operation scheduled a day later. My example of a failure to have a true employee in the mid-sized hospital in the Lexington-Mansfield Ohio hospital ED. I wish I had seen him again.
Yes, there is a shortage and the bad employees can thrive in such an environment.