Most Medicaid enrollees were unaware states can drop People “Now”
Fred Dobbs had a comment “a poll from KFF” on the Open Thread which led to this article. Read it, rewrote much of it, and posted it. More on the economics on healthcare. What is not being said here is what are the costs to the nation of no healthcare. Here we are just reporting on the disenrolled and not what is happening later.
“The Unwinding of Medicaid Continuous Enrollment: Knowledge and Experiences of Enrollees,” KFF, Multiple Authors.
Kaiser Family Foundation: During the COVID-19 pandemic, states kept people continuously enrolled in Medicaid in exchange for enhanced federal funding. Continuous enrollment in Medicaid ended on March 31, 2023. Over the coming months, states will redetermine eligibility for people enrolled in Medicaid and will disenroll those who are either no longer eligible or who are unable to complete the renewal process.
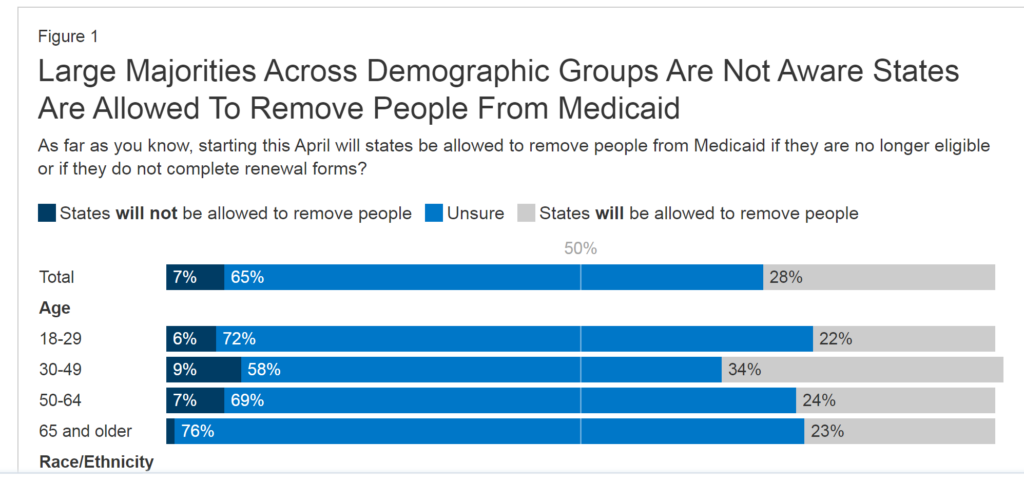
What appears to be prevalent in the disenrollment is most of the Medicaid enrollees were not aware states can now disenroll people from Medicaid. The keys to disenrollment are eligibility and being unable to complete the process. Many people were unsure states could now disenroll them. A small minority said states could not do this. Black adults were more likely than White adults to incorrectly say states will not be allowed to do this.
KFF’s Figure 1 reflects the numbers of and reasons for disenrollment.
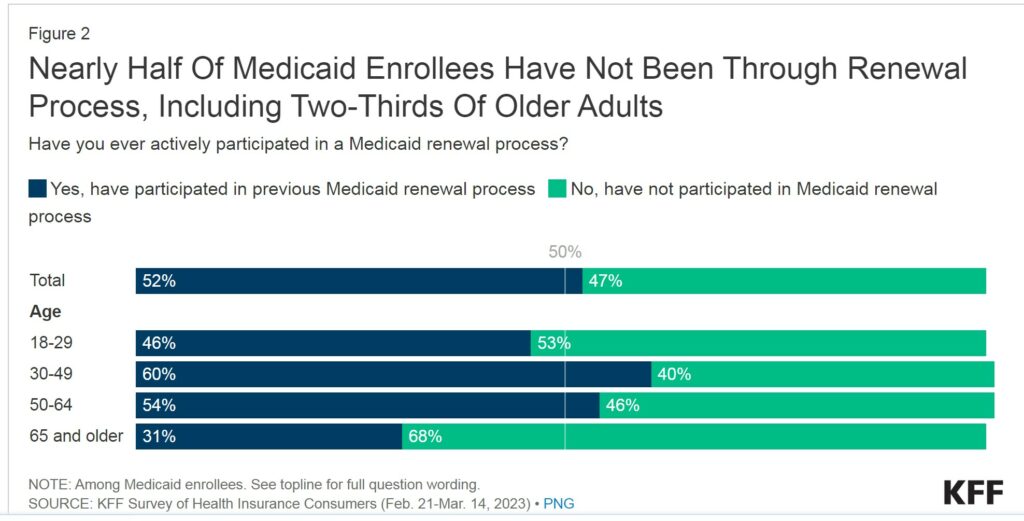
The kicker here (if I can paraphrase this issue) is nearly half of Medicaid enrollees being disenrolled had not been through a Medicaid renewal process in the past. They are “that” new to the process. Included in this administrative snafu are the “two-thirds (68%) of Medicaid enrollees who are 65 and older and the more than half of Medicaid enrollees who are between the ages of 18 and 29 (53%).”
Pre-pandemic Medicaid enrollee coverage was redetermined at least annually. Many lost coverage at renewal even though remaining eligible. Loss of benefits was due to administrative barriers to completing the process.
Why wouldn’t they be aware of a renewal process? Their Medicaid coverage was renewed because the state was able to complete the process using available data sources. The state did not require the enrollee to take any action to maintain coverage.
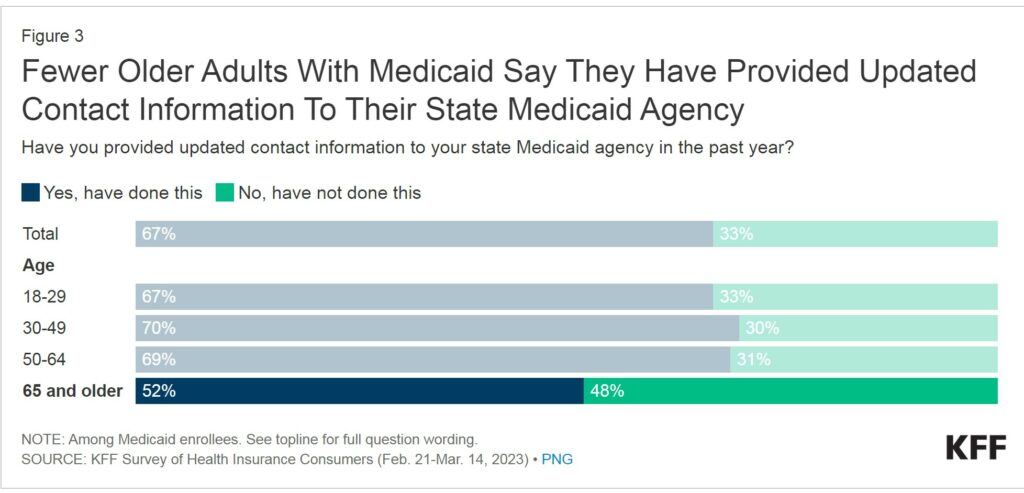
One-third of the Medicaid enrollees say they did not provide updated contact information to their state Medicaid agency in the past year. States have taken several steps in the past year to encourage Medicaid enrollees to update their contact information to increase the likelihood they would receive renewal information and other notices from the state. Two-thirds of Medicaid enrollees say they complied by providing updated contact information.
Older adults were more likely than younger age groups to say they have not provided updated contact information. Approximately half (48%) of those 65 and older did not provide the information. Older adults are more stable and consequently fewer need to report a change than other Medicaid enrollees. Also older adults are less likely to have either actively participated in a renewal process previously or provided updated contact information to Medicaid.
To add to the issue here, older adults prefer mail over other means of receiving information. For three-quarters of them, paper and USPS mail is the preferred method of getting information. Half of Medicaid enrollees prefer to receive renewal information through modes other than the USPS. The method being email or via an online portal. Except this manner of communication does not exist. There is also a chart on the KFF site also if you wish to see pictorial representation.
About one-third of Medicaid enrollees (35%) say they have had a change in income or other change, A change which could now make them ineligible for Medicaid. Or they are unsure if they have had such a change. Most enrollees say their circumstances have not changed and believe they are still eligible.
The numbers are not so great as to represent hundreds of thousands being dropped. One has to wonder if some states are in the mode of disqualification just to be mean-spirited. Some states like to discourage people through denial of healthcare, food, and subsidies. I can see this occurring in some states. Sixty-five percent of all Medicaid recipients said they had no changes. Twenty-five percent said they were unsure. Ten percent said they had a change.
In the end, disqualification for approximately six in ten of those on Medicaid as their only source of coverage would look for coverage from other sources if they were told they were no longer eligible. Over four in ten say they wouldn’t know where to look for other coverage or would be uninsured.
This is where a healthcare insurance expert source would be helpful. As Medicaid enrollees begin the renewal process, nearly nine in ten said having a state expert to help them navigate the process of renewing their Medicaid coverage and looking for other coverage, would be at least “somewhat useful.” Fifteen percent of disenrolled Medicaid insured say they would be uninsured if no longer eligible. Again someone to look for healthcare for them would be helpful.
A stronger version of providing help would be an advocate who could work the systems and gain healthcare for the uninsured. Understand, being uninsured or lacking coverage is some manner is more expensive. And the public will pay for the healthcare at potentially a higher cost.

Excellent healthcare post after post.
ltr:
This is off topic. If you wish to post something like this on Angry Bear talking about the new technology, I am happy to put it up.
Sorry, just delete the posts. Thank you.
https://www.nytimes.com/2023/05/26/us/politics/medicaid-coverage-pandemic-loss.html
May 26, 2023
Hundreds of Thousands Have Lost Medicaid Coverage Since Pandemic Protections Expired
As states begin to drop people from their Medicaid programs, early data shows that many recipients are losing their coverage for procedural reasons.
By Noah Weiland
Hundreds of thousands of low-income Americans have lost Medicaid coverage in recent weeks as part of a sprawling unwinding of a pandemic-era policy that prohibited states from removing people from the program.
Early data shows that many people lost coverage for procedural reasons, such as when Medicaid recipients did not return paperwork to verify their eligibility or could not be located. The large number of terminations on procedural grounds suggests that many people may be losing their coverage even though they are still qualified for it. Many of those who have been dropped have been children.
From the outset of the pandemic until this spring, states were barred from kicking people off Medicaid under a provision in a coronavirus relief package passed by Congress in 2020. The guarantee of continuous coverage spared people from regular eligibility checks during the public health crisis and caused enrollment in Medicaid to soar to record levels.
But the policy expired at the end of March, setting in motion a vast bureaucratic undertaking across the country to verify who remains eligible for coverage. In recent weeks, states have begun releasing data on who has lost coverage and why, offering a first glimpse of the punishing toll that the so-called unwinding is taking on some of the poorest and most vulnerable Americans.
So far, at least 19 states have started to remove people from the rolls….
https://fred.stlouisfed.org/graph/?g=GaXT
January 30, 2018
Medicaid benefits to persons as a share of Gross Domestic Product, 2000-2023
https://fred.stlouisfed.org/graph/?g=G49t
January 30, 2018
Medicaid benefits to persons as share of Disposable Income, 2000-2023
Hundreds of Thousands Have Lost Medicaid Coverage Since Pandemic Protections Expired
NY Times – May 26
Hundreds of thousands of low-income Americans have lost Medicaid coverage in recent weeks as part of a sprawling unwinding of a pandemic-era policy that prohibited states from removing people from the program.
Early data shows that many people lost coverage for procedural reasons, such as when Medicaid recipients did not return paperwork to verify their eligibility or could not be located. The large number of terminations on procedural grounds suggests that many people may be losing their coverage even though they are still qualified for it. Many of those who have been dropped have been children.
From the outset of the pandemic until this spring, states were barred from kicking people off Medicaid under a provision in a coronavirus relief package passed by Congress in 2020. The guarantee of continuous coverage spared people from regular eligibility checks during the public health crisis and caused enrollment in Medicaid to soar to record levels.
But the policy expired at the end of March, setting in motion a vast bureaucratic undertaking across the country to verify who remains eligible for coverage. In recent weeks, states have begun releasing data on who has lost coverage and why, offering a first glimpse of the punishing toll that the so-called unwinding is taking on some of the poorest and most vulnerable Americans.
So far, at least 19 states have started to remove people from the rolls. A precise total of how many people have lost coverage is not yet known.
In Arkansas, more than 1.1 million people — over a third of the state’s residents — were on Medicaid at the end of March. In April, the first month that states could begin removing people from the program, about 73,000 people lost coverage, including about 27,000 children 17 and under.
Among those who were dropped was Melissa Buford, a diabetic with high blood pressure who makes about $35,000 a year at a health clinic in eastern Arkansas helping families find affordable health insurance. Her two adult sons also lost their coverage.
Like more than 5,000 others in the state, Ms. Buford, 51, was no longer eligible for Medicaid because her income had gone up. A notice she received informing her that she did not qualify made her so upset that she threw it in a trash can.
But a majority of those who lost coverage in Arkansas were dropped for procedural reasons.
Daniel Tsai, a senior official at the Centers for Medicare and Medicaid Services who is helping to oversee the unwinding process for the Biden administration, said that more outreach was needed to help those who lost coverage that way. He said federal officials were in regular contact with state officials around the country to review early data on the unwinding and check whether people who lost coverage had a fair shot to prove their eligibility.
Gov. Sarah Huckabee Sanders of Arkansas, a Republican, has framed the unwinding as a necessary process that will save money and allow Medicaid to function within its intended scope. …
Reply
Fred C. Dobbs says:
May 27, 2023 at 8:53 am
In some states, hundreds of thousands dropped from Medicaid
NPR – May 24
States have begun to remove people from Medicaid, something they could not do for three years during the COVID-19 pandemic.
State Medicaid programs are reviewing the eligibility of roughly 90 million beneficiaries in the U.S., now that a rule suspending that process has expired. Those who remain eligible should be able to keep their coverage, and those who don’t will lose it.
But new data from states that have begun this process show that hundreds of thousands of people are losing coverage – not because of their income, but because of administrative problems, like missing a renewal notification in the mail.
And a poll this week from KFF found that 65% of Medicaid enrollees across the country didn’t know states can now remove people from the program if they are not eligible or don’t complete the renewal process. …
Reply
Fred C. Dobbs says:
May 27, 2023 at 8:55 am
a poll this week from KFF
Reply
And a poll this week from KFF found that 65% of Medicaid enrollees across the country didn’t know states can now remove people from the program if they are not eligible or don’t complete the renewal process. …
Reply
Fred C. Dobbs says:
May 27, 2023 at 8:55 am
a poll this week from KFF
Reply
from post on ‘Expanding the role of Medicare in US healthcare’