Healthcare Costs and Its Drivers Today
I have been doing my typical reading on healthcare in the US and ran across several articles which seemingly come together at various points in the dialogue and are written by different authors. I decided to tie them together into a much wider and telling story.
An interesting point being was made by MedPage Today’s Dr. Milton Packer on his blog, “people suffer and die because Payors (Healthcare Insurance) is cost effective.” He starts his discussion on the opiate epidemic in the US, opiates are being prescribed by doctors for pain relief and . . .
“Patients are becoming addicted to opiates after the initial 10 day prescription with one-fifth of patients still using opiates a year later. There is no need to prescribe opiates as other less addictive pain-relief formulations are available, which are not commonly prescribed.” This raises the question of why?
Payers will not pay for the alternatives. The less-addictive opiates are more expensive and payers have declined to support them. Patients get addicted because prescribing for the lower cost and highly addictive opiates saves the payers money initially (me).
September 17, 2017, the New York Time and ProPublica (independent, nonprofit investigative journalism organization) collaborated on an article concerning the opiod epidemic in the US.
At a time when the United States is in the grip of an opioid epidemic, many insurers are limiting access to pain medications that carry a lower risk of addiction or dependence, even as they provide comparatively easy access to generic opioid medications.
The reason given: Opioid drugs are generally cheap while safer alternatives are often more expensive.
While the pharmaceutical manufacturers, distributors , and doctors have come under scrutiny; insurance companies and the pharmacy benefit managers (CVS Caremark, Express Scripts and OptumRx) make the final decisions as to what is covered. It could be something as simple as a higher tier and deductible to block usage.
A little side trip here and a continuation of the above. A week or so ago, I ran across another MedPage Today article by Dr. Packer; “ Who Actually Is Reviewing All Those Preauthorization Requests and How the System Works.” Dr. Packers was giving a talk on advances in medicine with regard to heart failures to a room of about 20 or so doctors who were retired.
Since many of them were no longer involved in active patient care, he wondered why they might want to hear a presentation on new advances in heart failure. Here was their answer:
Doctors: “We no longer care for patients, but we care about what’s going on. You see, most of us are employed by insurance companies to do preauthorization for drugs and medical procedures.”
“Dr. Packer: I just gave a talk about new drugs for heart failure. Are you responsible for preauthorizing their use for individual patients?”
The answer; “Yes.”
“So did I say anything today that was helpful? I talked about many new treatments. Did I say anything that you might use to inform your preauthorization responsibilities?”
“Oh, we’ve heard about those drugs before. We are asked to approve their use for patients all the time; but, we don’t approve most of the requests. Nearly all of them are outside of the guidelines we are given.”
“I just showed you evidence that these new drugs and devices make a real positive difference in people’s lives. People who get them feel better and live longer.”
“Yes, you were very convincing. But the drugs are too expensive. So we typically reject requests, at least the first time. We figure that, if doctors are really serious, then they should be willing to make the request again and again.”
“If the drugs will help people, how can you say no?”
“You see, if it weren’t for us, the system would go broke. Every time we say yes, healthcare becomes more expensive, and that isn’t a good thing. So when we say no, we are keeping the system in balance. Our job is to save our system of healthcare.”
“But you are not saving our healthcare system. You are simply making money for the company that you work for. And patients aren’t getting the drugs that they need.”
“You really don’t understand, do you? If we approve expensive drugs, then the system goes broke. Then no one gets healthcare.”
“Plus, if I approve too many expensive drugs, I won’t get my bonus at the end of the month. So giving out too many approvals wouldn’t be a smart thing for me to do. Would it?”
Now before you start on insurance companies and doctors; understand, this is not as free a market place as many would assume. In all of their political wisdom, Congress favors pharmaceutical companies over doctors, insurance companies, and the welfare of the constituents. Through legislation, Congress has made it impossible for insurance companies to negotiate pharmaceutical pricing in Medicare Part D insurance and also the ACA. Furthermore with the consolidation happening in healthcare, negotiation by insurance companies with a consolidating and growing healthcare industry is becoming more and more difficult as the former does not have as great of leverage. You have read my argument calling out of Single Payor, Medicare-for-All, Public Option, etc. as the cure for today’s healthcare issues and rising cost not being enough as the ACA and Part D were specifically blocked or the cost issue unaddressed in the legislation written by Congress. If these issues are not addressed from the very beginning, we will be fighting the same issues with rising costs a decade later with other programs.
At this point, I begin to disagree with Dr. Packers as he goes on to say:
“So we spend more for healthcare than any other country in the world; but, Americans do not get the care they need. There is a simple reason. Treatment decisions are not being driven based on a physician’s knowledge or judgment. They are being driven by what payers are willing to pay for.”
It is true that patients may not get some of the healthcare they need at the time due to denial, which can be appealed to the ACA, and can be a tiring process. It could be approved, passed on to patients, resulting in higher premiums the following year, and the Part D Risk Corridor program pay for it if excessive for the present year. What Dr. Packers does not mention is the rising prices and cost of drugs being blamed by pharmaceutical company on R&D, tooling up to manufacture, etc. The counter argument is much of the R&D is funded by the US government through tax deductions and write-offs for pharmaceutical R&D and capital Overhead. Pharmaceutical profits are double digit at ~25% beating out hospital supplies and healthcare insurance, which is already limited in what can be charged back to the insured by the MLR. To blame insurance companies totally for the higher costs in healthcare is false. Furthermore, a doctor’s decision do not always lead to less costly cures or practices.
Maggie Mahar of Health Beat Blog would take the subject of costs a step farther and state Medicare will approve anything the FDA approves for usage regardless of the quality of outcome when measured against older proven treatments. Notably the VA does limit its pharmacy and its care is rated higher than that of today’s commercial, for-profit healthcare to which most citizens are exposed.
Dr. Donald Berwick, President Obama’s proposed appointment for Medicare and who was in charge of Medicare and Medicaid for 17 months stated;
“20 to 30 percent of health spending is ‘waste’ that yields no benefit to patients, and that some of the needless spending is a result of onerous, archaic regulations enforced by Medicare and Medicaid.
He listed five reasons for what he described as the ‘extremely high level of waste.’ They are overtreatment of patients, the failure to coordinate care, the administrative complexity of the health care system, burdensome rules and fraud.
Much is done that does not help patients at all and many physicians know it.”
That is the same Medicare/Medicaid being touted by many proponents today as an alternative.
Speaking of costs and pricing for pharmaceuticals, there have been recent incidents of skyrocketing costs on particular drugs. A short while ago, I wrote a post concerning the appointment of Alex Araz as the new HHS Secretary replacing Dr. Tom Price. Formerly, Alex Araz was the CEO of the pharmaceutical giant Eli Lilly & Co.’s U.S. division. He also served under George W. Bush administration as the HHS General Counsel and Deputy Secretary. During that stint, he received praise for his management competence with the HHS; although, he did not have a healthcare background prior to this position.
Here it gets interesting when examining what took place during his tenure with Eli Lilly. One of the leading costs identified in pharmaceuticals increases has been in the rising cost of diabetes medication.
“While the Tweeter-in-Chief, Trump tells us presidential campaign contributor Alex Azar will be a ‘star’ who will lower prescription prices,”
Public Citizen’s Peter Maybarduk (Director) had this to say: “Eli Lilly is notorious for spiking prices of a century-old isolated hormone during Azar’s tenure as president and vice president. Eli Lilly raised the price of Humalog by 345%, from $2,657.88 per year to $9,172.80 per year.
Maybe President Trump in appointing Alex Azar to be HHS Secretary should have asked the 6 million diabetic Americans whose insulin prices have more than tripled under Azar’s watch at Eli Lilly.”
This has nothing to do with R&D and has more to do with pharmaceutical companies controlling the market regardless of supply and throughput restricted manufacturing (capacity).
What I have tried to do is tie these articles together into one cohesive story of how the pharmaceutical industry, insurance, and healthcare can have an impact on healthcare costs. For those who are interested, my background does include working in the manufacture of hospital supplies and pharmaceuticals. Using various citations from these articles, I have tried to touch upon the impact of insurance companies, the healthcare industry, government intervention under the HHS, one particular Med in the market place, etc. Overall, what is going on in the marketplace.
Another article, I read the other day gets into the foundation of what is happening based upon a recently completed study by JAMA. Using this study, the Methods Man, Dr. Perry Wilson (MedPage Today) examines what is driving healthcare costs in his article Here’s What’s Really Driving Healthcare Costs using data from Factors Associated With Increases in US Health Care Spending, 1996-2013 and the US Disease Expenditure Project. Dr. Wilson breaks it down using three simple charts which I have consolidated to one.
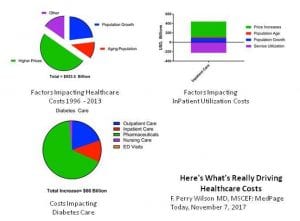 Dr. Perry Wilson starts off making an overall point about the rising cost of healthcare from 1996 to 2013 and stating; “after accounting for inflation, healthcare expenditures increased $933.5 billion from 1996 to 2013.”
Dr. Perry Wilson starts off making an overall point about the rising cost of healthcare from 1996 to 2013 and stating; “after accounting for inflation, healthcare expenditures increased $933.5 billion from 1996 to 2013.”
Going on: “Healthcare expenditures in the US being high and rising rapidly is nothing new, but the study appearing in the Journal of the American Medical Association identifies the exact components of healthcare that are driving those soaring costs. The data from this study suggests traditional economic forces break down in the US healthcare market.
Different chronic diseases have different patterns of price increases. The biggest increase was seen in diabetes care, as you can see here, driven largely by the rising costs of pharmaceuticals.”
The Chart breakdowns reveal the various impacts of healthcare costs moving from left to right and then downward:
• 50% of the increase in healthcare costs was simply due to higher prices.
• Inpatient care or Service Utilization (purple) went down from 1996 – 2013 as outpatient treatment increased; however, the price of the remaining inpatient care went up much more – increasing overall inpatient care spending by around $250 billion.
• Different Chronic Diseases have different patterns of price increases. The biggest increase was seen in diabetes care and driven largely by the rising prices of pharmaceuticals.
The takeaway drawn by Dr Perry Wilson: “Regardless of the disease, it is clear, the price of what we’re buying – whether a drug, an ED visit, or a hospital stay – not the amount of what we’re buying is the major driver of cost increases. Efforts to reduce the consumption of healthcare may not bend the cost curve as much as efforts to reduce its price.”
You can not make an argument about the regulation of costs “not” being one of the dynamic components of a healthcare plan given the continuous unhindered industry driven rising cost of healthcare. Yet, every healthcare plan I have read fails to mention cost regulation specifically, provide remedy for it, and many assume a natural occurrence of control.
by run75441 (Bill H)

Run thanks for this, but in my opinion you’re avoiding the central problem , though you briefly touched upon it without being more explicit:
“This has nothing to do with R&D and has more to do with pharmaceutical companies controlling the market regardless of supply and restricted manufacturing throughput. ”
The market can’t be controlled by the pharmaceutical companies unless the government lets them. So this is a government sourced and caused problem unless you believe laissez-fair is the gov’ts job to promote and endorse.
You can’t blame the pharmaceutical companies for doing precisely what the gov’t lets them do by law.. the pharmaceuticals company’s owners are in this to be philanthropic are they?
What you are essentially not coming to grips with is that our government is not designed to be democratic but designed by it’s concept to be a system to ingratiate those who pay the most to keep the gov’t in power which is to say those that represent them are paid to do their bidding… in other words a gov’t controlled by the sources of wealth to maintain it. if it were anywhere near a democratic system, how could 1% control it?
Run, sorry … I forgot that there’s never been a democratic system from the Spartan through the Athenian to the present that hasn’t been controlled by the wealth. There have only been moments brought about by extreme deprivation that have had to deal with that deprivation to avoid revolution.
When we want to fix U.S. healthcare costs and quality we know how to do it, but you have to fix the system of government we employ to do it. Address the source of the problem rather than effects of it.
Run, let me only add that I don’t know how we can have a free market based and biased system of government and anything even approximating a democratic system at the same time. That is the actual dilemma since they are mutually exclusive.
If you think about how to “comprise” one with the other then you have to decide how such compromise is made and sustained (sustained being key word) and I can’t see or find any evidence in U.S. history that suggests such compromise has ever worked to provide for the greater good on a sustained basis.
Perhaps its not even possible among human systems of civilized government .. but then why the charade as if it is? If the public wants to improve the healthcare system then why does it elect Presidents and representatives who don’t want to improve it? If the public want’s to improve the healthcare system why do Supreme Court interpret the Constitutional “law” to prevent it? Or if the 200+ year old constitutional law is so outdated as to be irrelevant than why doesn’t the pubic demand to change it?
Or does the pubic want it’s cake and eat it too? The public may be confused (I’m sure of this in fact) because they want simultaneously mutually exclusive conditions.
Run, great major post.
Long, “… I don’t know how we can have a free market based and biased system of government and anything even approximating a democratic system …”
No? Look at continental Europe — look at across the board labor union density — look at sector-wide labor agreements. Come to think look at our northern neighbor.
Mostly all other problems from health care to student debt to everything are just symptomatic of the same economic/political-union free pathology. Bernie and Eliz don’t spend a lot of time looking abroad either — or even looking at 1973 stateside.
Come a Dem Congress I think the best idea is:
Why Not Hold Union Representation Elections on a Regular Schedule?
Published November 1st, 2017 – Andrew Strom
This can be sold as taking a page from Repub govs (e.g., Walker) who force government employee unions to re-certify every year — with majority of union members, not just those who vote, required to retain.
I’m playing with the idea of proposing (via spam mail*) re-certification for every union in the country every year — oh, of course, that would include certification elections for every nonunion workplace: that’s the Trojan Horse.
We really want to certify/recertify every three or five years (three at first while we are trying to build density — maybe five later on). Once we organize enough we can write the rules any way we want. By proposing re-certification every year (from my spider hole in Chicago) maybe I can get union members dander up and thereby at least wake them up to the issue. Cab driver political drama.
(* I have about 2000 email addresses, journalists, union, academic, politicians — in WA, OR, CA, NV — that I like to hit with new ideas.)
Denis:
You may want to look at this again. A portion of it was blocked due to an error in linking to an article on Pharma costs which was kind of important. I have another article coming out which will discuss Pharmaceutical companies pulling advertising from medical news sites and mags if they are critical of pharma. As I read each of these articles, I could see a similar thread in them.
in 2015, AARP broke ties with MetLife over LTC insurance which MetLife discontinued in 2011 (no new applications). No big deal except AARP never told its membership of the AARP sponsored insurance break with MetLife. AARP now has a new LTC insurer New York Life announced as of 2015 and no letter to its members holding MetLife policies. Those who had AARP sponsored MetLife are now left with MetLife who is requesting a 21.75% increase just for cost over 3 years in addition to the normal inflation factor which was ~10% for 2018. AARP refers all inquiries to MetLife even though documents from MetLife still has AARP logos on it. Another interesting post of companies and Organizations screwing people.
Dennis,
FWIW I come from a long line of union activists, members, and in one case a major union leader in the western U.S. and California in particular — Building & Construction Trades Council.
I’ve been and remain a hugely strong union supporter. However my uncle (the Western US major union leader) was a realist and well understood the nature of economics viz-a-viz unions and capital owners.
In a series of discussions while I resided with he and his wife during one summer college break, he made me understand those trade-offs, and what drove them. At the time the college educated workforce in the US was 10% (4 year or better degree). He said a major factor in union’s was the level of the college educated workforce and he said in 1966, that if the rate of college degree growth reached the then unprecedented rate of ~ 0.5%/year than in a few decades 1/3rd of the workforce would have college degrees — the upshot of which is that they would very unlikely be persuaded to join unions or create new ones. His prognosis in 1966 turns out to be pretty close to reality even though he had little historic information to go on., .. he was not a pie in sky type, but a practical and major proponent of the general working class an working poor.
He also told me in 1966 that if unions demanded too much of the capital owners profits, they would resort to capital invested in automated methods — his primary example of which was the hift to lath & plaster skilled union members to wall board … which required no skill per-se and that forced union wages for interior “plasterers” down as lower skill and more efficient “sheetrock” hangers too over.
He cited other examples of automation replacing skilled union labor and without elaborating it was an eye-opener for me to see that unions were on their way down He not only knew the economics of building and construction business and labor, but of mining and manufacturing.
This was all long before Reagan’s anti-unionism push (which in reality was Reagan using what was already well underway as a means of pumping up is conservative credentials).
My uncle’s wisest advice was that if unions demanded more than capital owners were able to profit, they would simply use their capital in other enterprises where profits were greater — this included not only investing in automated methods in mfg’ing and the building and construction trades (remember “sheetrock”) , but in foreign low wage labor regions where especially mfg’ed goods could be produced at lower costs IF(the big IF in 1966) transportation and import duties made it more profitable to do so. He cited Mexico as the primary source of low transport cost low wage labor at the time, and at that time import duties from the few mfg’ed goods produced in Mexio were excessive which was the only reason mfg’ing hadn’t shifted to use Mexican labor in Mexico for production and also why mfg’ing was investing more and more capital in automation. BUT, he said sooner or later it would become clear that capital owners would push to chane US import policies from Mexican roduced goods and the this would reduce mfg’ing’s need for U.S. labor, thus Union’s would have far less leverage to take a share of capital profits.
So he was a few decades off in his estimates, but he was right in 1966.. My uncle was among those in the U.S. union leaders who all understood all this very well… what they said in public was different that what they saw occurring and would continue to occur … they just didn’t know then the rate of occurrence — the computer age hadn’t started …. semi-conductors were being invented and barely developed for example. China’s opening up hadn’t occurred yet either. Clinton’s NAFTA was still far in the future.
Through al the years since 1966 I’ve watched the progression of what my Uncle told me during our discussions in the summer of 1966. take place, for precisely the reasons he (and other major union leaders) knew they would.
In hindsight what fails in the U.S. relative to Europe is Germany’s constitutional protections of labor unions. which by osmosis transfers to the other major European nations…just as U.S. union wages and benefits transferred by the same osmosis to non-union wages and benefits rising to keep pace.
Keep up the good fight, Dennis, but you’re forgetting about the economic realities in the US and it’s individualism worship and constitution that protects it. .
Run, as you know, nothing substantive on controlling medical costs can possibly occur with Republicans in charge. With Democrats in charge, it’s tough enough. Witness the ACA’s development and the impact of the blue dogs.
JackD wrote “Run, as you know, nothing substantive on controlling medical costs can possibly occur with Republicans in charge.”
I could not agree with you more.
The Republicans’ implementation of Medicare Part D which forbids negotiation of drug prices was asinine. Where was their concern for the national deficits and debt?
On heath care President Obama was negotiating with the duplicitous. His opposition had only one concern, their oath to Grover Norquist.
It’s not just that pharma has some say on what gets published, but in the health literature world, the trend was to only publish positive results.
As you can imagine, this has left a major void in truly understanding what happens in the body when a treatment is applied. There is a push to change this. Additionally, there is the push toward the idea of “numbers to treat”. That is, how many have to receive the treatment to create one positive results. Outcomes can look a lot more different when looking at numbers to treat.